Payers are pulling ahead. Here’s how to catch up — and take the lead.
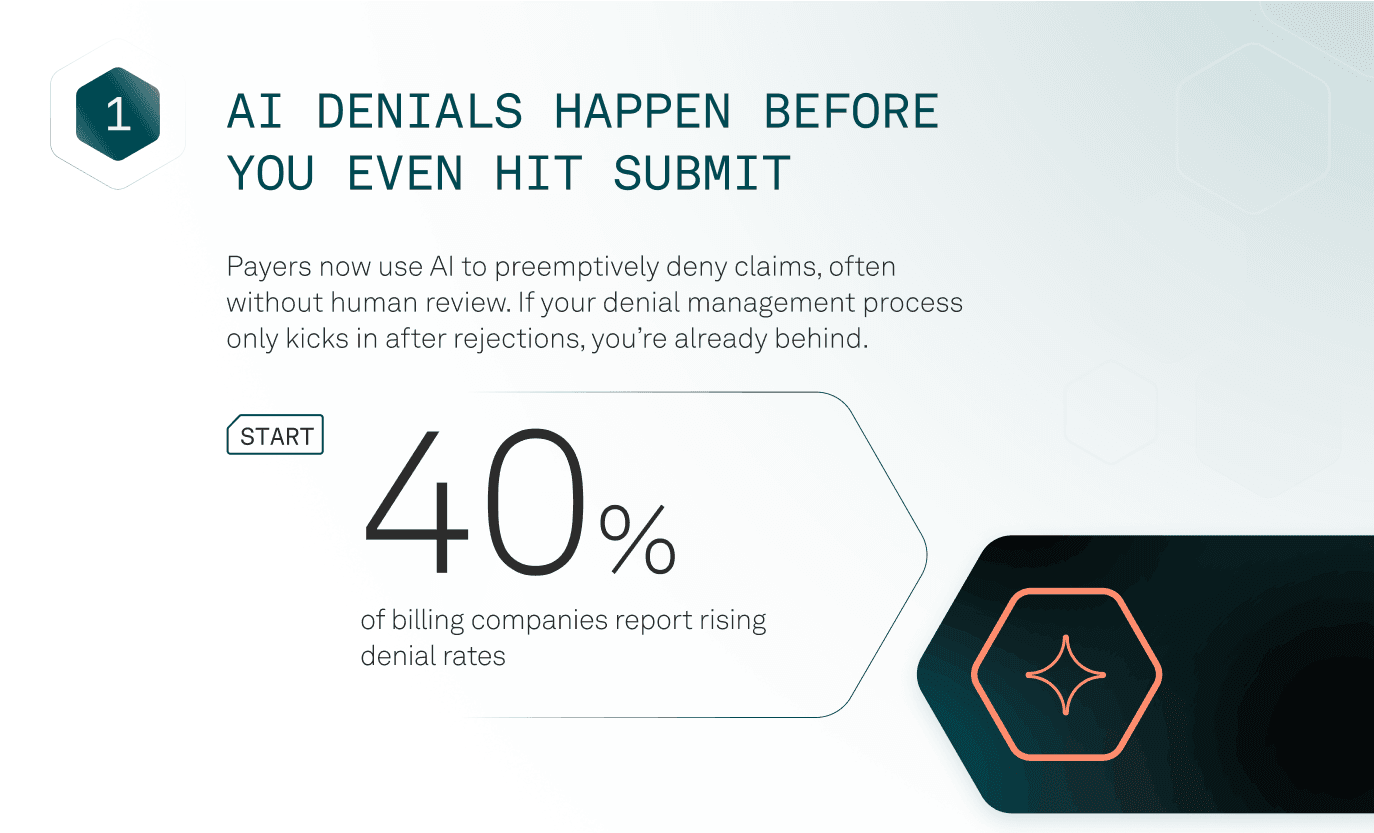
Payers are speeding up denials and slowing down reimbursements — using AI, automation, and airtight compliance to shift the burden to billing teams. But you’re not powerless.
This free guide reveals 5 payer strategies and what leading billing teams are doing to protect revenue, cut rework, and take back control.

Get a sneak peek

Outsmart payers — no overhaul required
Payers have changed the game. Too many billing companies are stuck reacting. This guide helps you:
- Catch AI denials before they happen
- Automate critical steps — no overhaul required
- Turn compliance into a competitive edge
- Flag delays before they cost you
- Compete with payer-level data — no data team needed
If you’re relying on rework and reaction, this is your sign to upgrade.
Reclaim control — without burning out your team
Download your FREE guide nowBilling companies that adapt fast don’t just survive — they gain ground.
With the right tools and tactics, you can:
- Slash manual work and rework
- Accelerate reimbursements
- Build resilient workflows that resist payer pressure
This guide gives you the edge to scale with less stress — and lead with confidence.
Still have questions?
It outlines 5 strategic shifts payers are making — and gives you practical ways to respond and recover lost revenue faster.
Billing company owners, revenue cycle managers, and operational leads who want to stay competitive in today’s payer-dominated environment.
Not at all. Whether you’re just getting started or already exploring automation, this guide helps you take the next step strategically.
Yes — no strings attached. Just expert-backed tactics from the Tebra billing and RCM team.
You can always connect with our team or explore more tools in the Tebra resource center.