Reduce denials & get paid faster — turn rejections into revenue
Denials are rising, with 12% of claims denied in 2024 and 40% of billers reporting an increase in rejection rates. Every delayed or lost claim affects your revenue cycle — but you don’t have to accept them as lost income.
This free guide breaks down five fast fixes that help medical billers triage, resolve, and prevent denials faster — reducing turnaround times and increasing approvals.

Get a sneak peek

Five fast fixes for faster payments
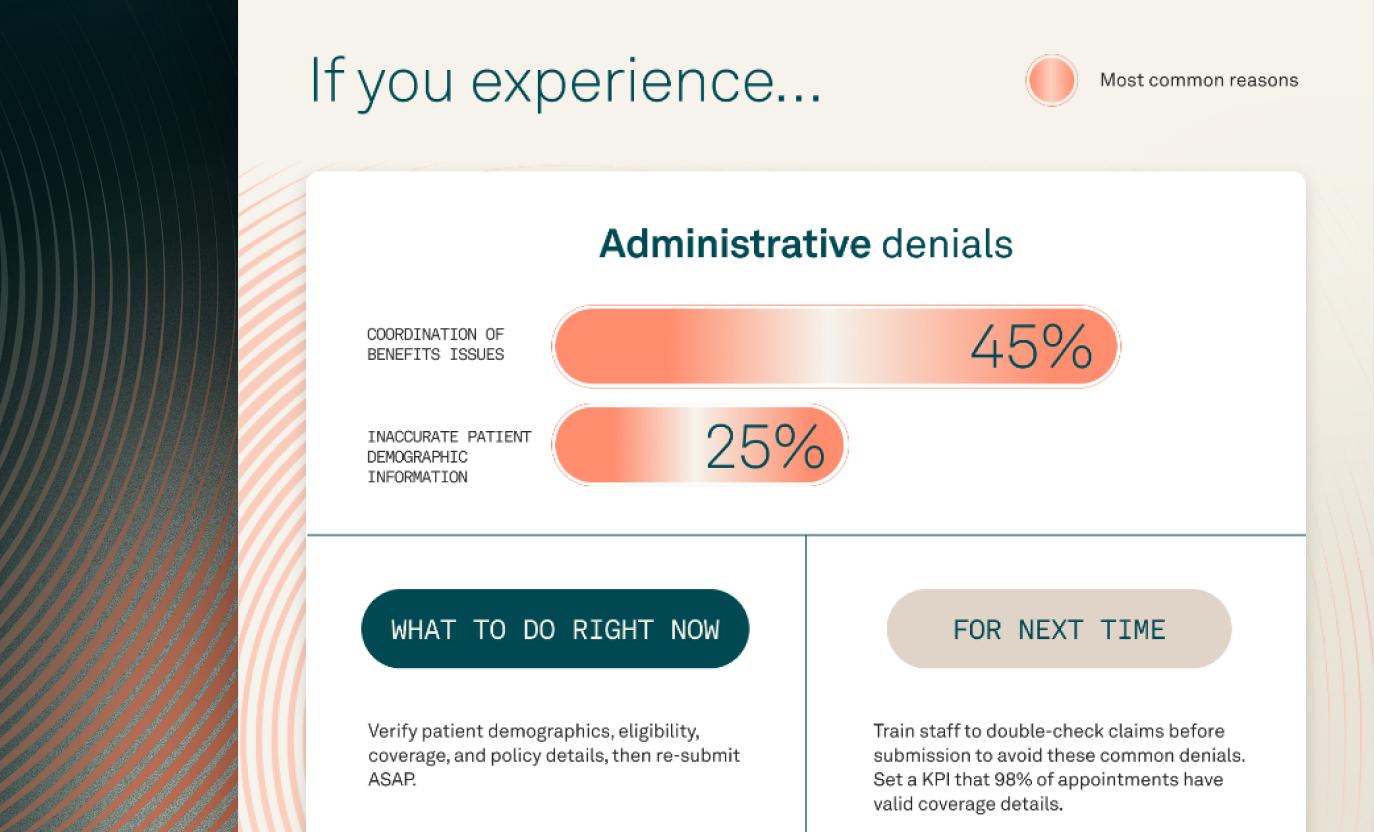
Denials don’t have to disrupt your revenue cycle. A recent Tebra survey found that the most common reasons for claim denials include coordination of benefits issues (45%), noncoverage (39%), and prior authorization errors (31%) — all of which can be prevented.
This free guide gives you the blueprint to:
- Eliminate preventable denials with staff training and automation
- Accelerate appeals by standardizing processes and tracking KPIs
- Reduce errors with payer-specific coding and documentation best practices
- Improve claim accuracy so more approvals happen on the first submission
Stop leaving money on the table — take control of your denials today.
Reduce denials, recover revenue — here’s how
With the right system in place, you can:
- Automatically flag denials before they impact cash flow
- Use AI-powered tools to categorize, track, and triage denials instantly
- Implement standardized processes that increase approvals and minimize delays
Still have questions?
Download this guide and Take control today.