System integration strategies for medical billers
Billing companies face growing pressure to work inside multiple client systems — each with unique challenges. This guide shows you how to set guardrails, price for complexity, and automate key steps so more claims run hands free and cash moves faster.

Get a sneak peek

Why multi-system workflows leak margin
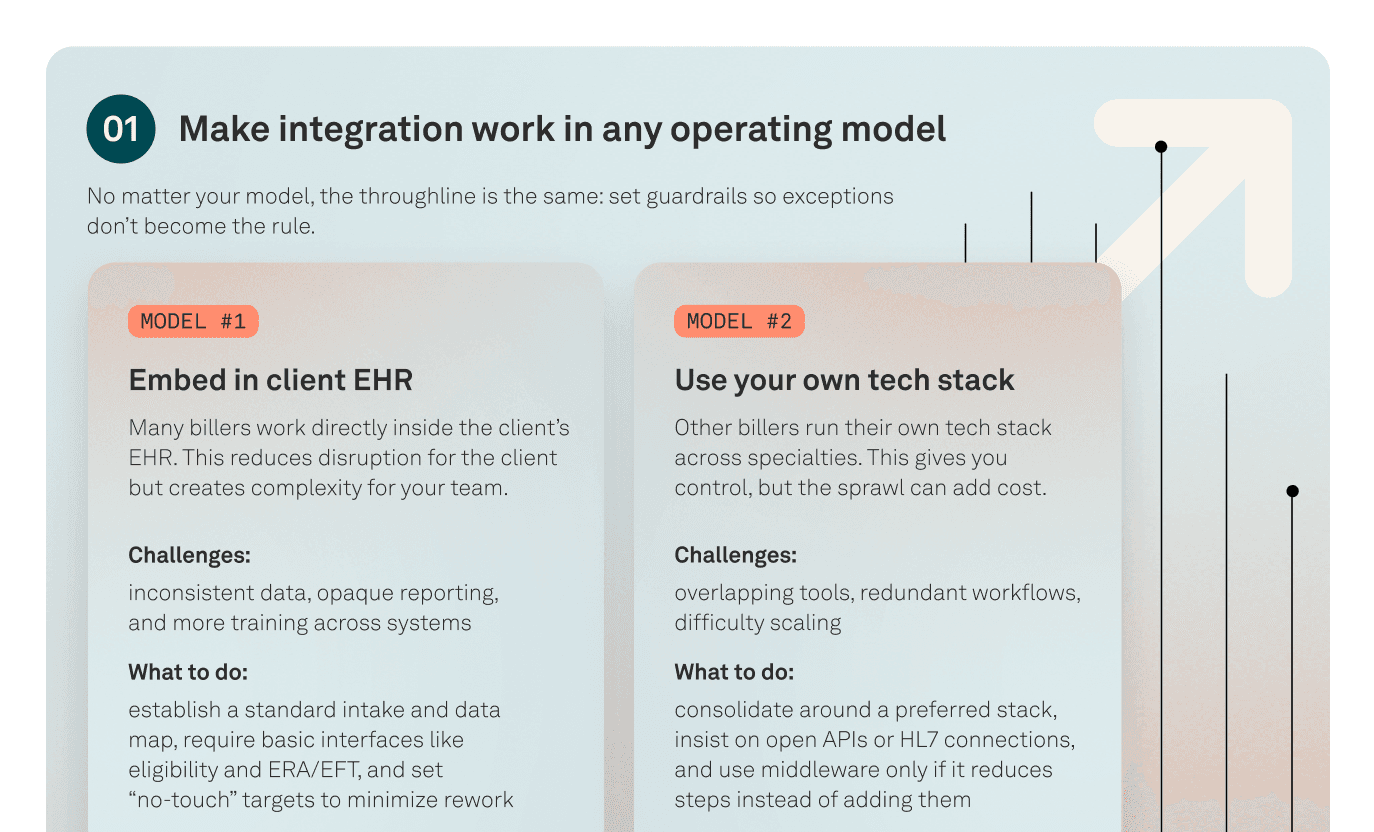
Working in multiple client EHR/PM systems creates extra touches, inconsistent data, opaque reporting, and slower cash flow. In embedded setups you lose visibility; in stack-owner setups you risk overlapping tools and redundant workflows.
This guide will show you how to:
- Set guardrails and price for complexity so exceptions don’t become the rule
- Standardize intake and data maps and require eligibility and ERA/EFT interfaces
- Prefer open APIs or HL7 and use middleware only when it reduces steps
- Automate high-impact steps like eligibility, claim creation, ERA posting, and statements
Train continuously, capture front-line insights, and track an operations scorecard
Make system integration your advantage
Get the FREE guideIntegration delivers results when you set clear guardrails, standardize data, and automate the right steps. These practices reduce touches, prevent errors, and keep cash moving.
- Standardize intake and data maps across client EHRs and PMs
- Require core interfaces like eligibility and ERA/EFT to cut manual work
- Prefer open APIs or HL7, and use middleware only when it removes steps
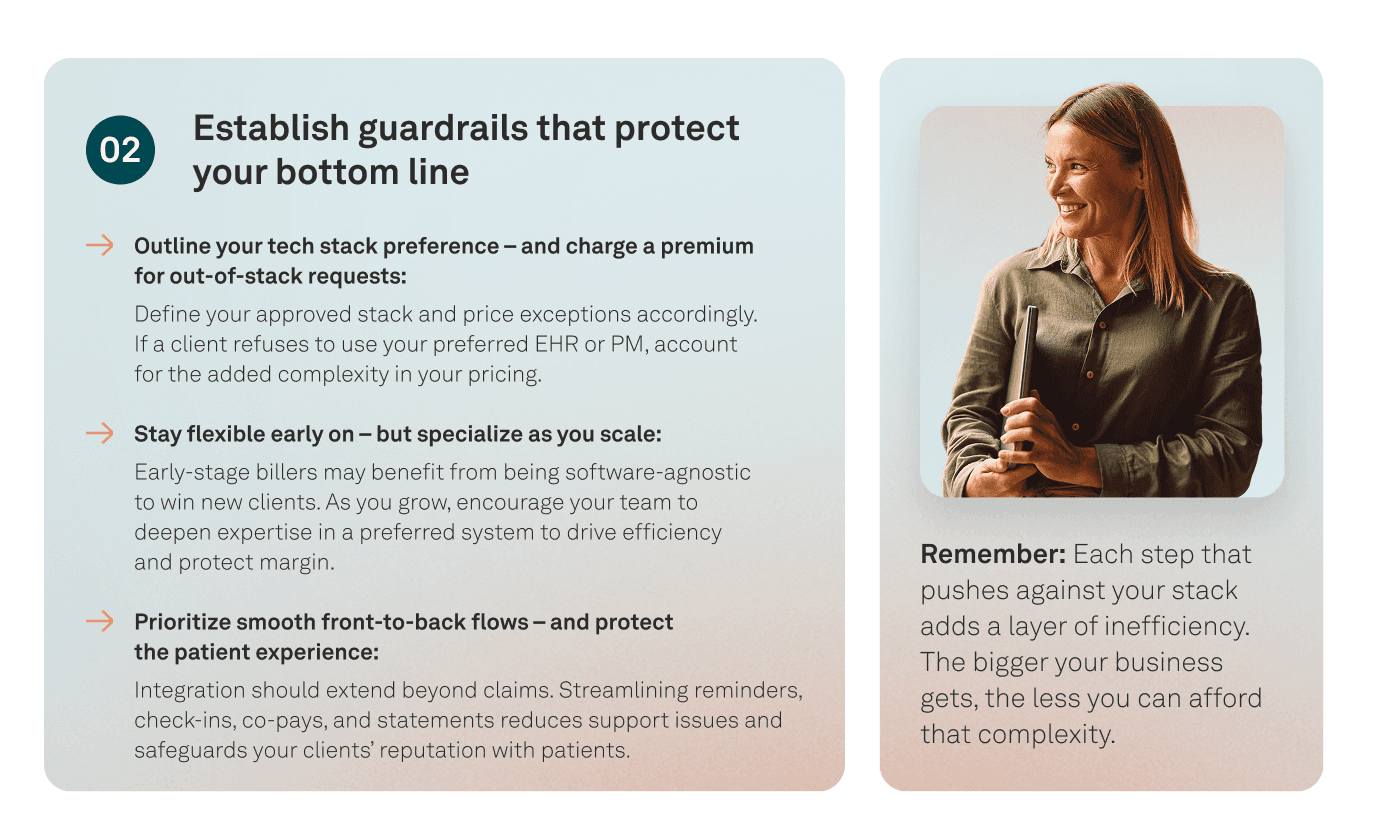
- Price for complexity so out-of-stack requests do not erode margins
- Automate high-impact tasks: eligibility, claim creation, ERA posting, statements