
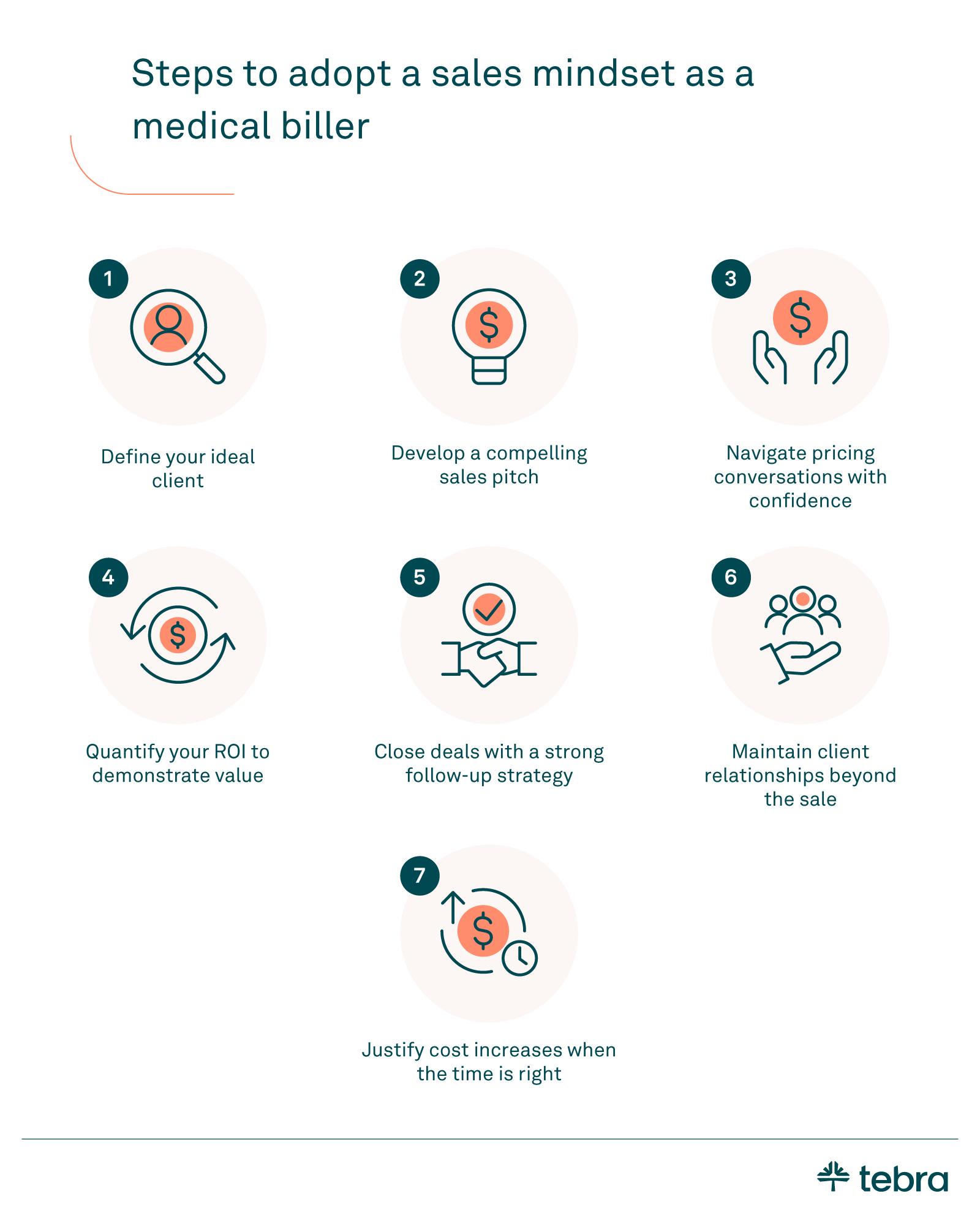
- Adopt a consultative approach that helps medical practices in healthcare see clear ROI, supported by metrics and success stories.
- Define the ideal customer, build data-driven pitches, and keep consistent follow-up so providers understand value and next steps.
- Sustain regular engagement and proactive service, and align work with strong revenue cycle management to secure long-term partnerships and growth.
Medical billing companies excel at streamlining revenue cycle management (RCM) and ensuring timely reimbursements through accurate healthcare billing. Yet, many medical practices hesitate to outsource medical billing services due to budget concerns or unclear value.
A sales-oriented approach helps billers translate outcomes for providers, connect the work to day-to-day practice management, and position themselves as strategic partners in the medical billing industry. It also fits more naturally alongside modern EHR software.
Follow these tips to hone your skills as a medical biller and win more business.
1. Define your ideal client
These tips can help you build an ideal customer profile (ICP):
- Identify key characteristics: Determine the types of practices that benefit most from your services. Look at practice size, patient volume, current billing challenges, and financial health. Tie these details back to day-to-day practice management needs.
- Align your solutions with their needs: Map common pain points to clear outcomes. If denied claims or slow reimbursements are common, show how your workflows reduce errors and speed collections. Explain how your medical billing business supports staff and leadership with simple reporting.
- Name segments and demand channels: Define your target market by specialty and growth stage. Include areas such as physical therapy. Plan how to reach new clients through qualified leads and referrals, plus simple outreach that fits your team.
Example: If a practice struggles with administrative overload, emphasize how your processes and tools lower backlogs and increase collections. Share a short story that shows measurable time savings and fewer errors.


"If a practice struggles with administrative overload, emphasize how your processes and tools lower backlogs and increase collections."
2. Develop a compelling sales pitch
Here's how to craft your value proposition to potential customers.
- Focus on differentiation: Highlight what makes your billing company unique. Whether it's specialized expertise, modern tools, or proven results, make sure your pitch clearly shows the edge you bring as part of a clear marketing strategy. Align messaging so your sales team and salespeople present the same promise across calls, email, and meetings.
- Use data to build credibility: Incorporate statistics or success stories to back up your claims. Share concise case studies, pull short testimonials, and offer lightweight white papers on LinkedIn to reinforce results. Point out who will do the work. If a medical billing specialist leads the account, say so.
Example pitch: "We have been experts in this specialty for over 15 years and have helped hundreds of practices speed up their revenue cycle. Here is how we can achieve the same for you."
Practice your pitch regularly
Run role-playing exercises with a colleague to refine clarity, tone, and objection handling. Keep a living list of common objections with calm, value-based replies. Adjust delivery for phone, video, or in-person meetings, and decide which content marketing assets support your point, including visuals or brief narratives.
Supporting materials: Accurate medical coding and correct use of CPT and ICD-10 signal quality. Proof of credentialing status and payer enrollments helps reduce friction. Bring brief exhibits that show how your process avoids errors and speeds clean claims.
3. Navigate pricing conversations with confidence
When costs come up, budget worries are normal. Use the ARA approach (acknowledge, respond, ask) to keep the conversation clear and helpful.
Acknowledge: "I understand that budget is a concern."
Respond: "Our work improves collections and speeds reimbursement. We account for your payer mix, including Medicare and commercial health insurance, so revenue impact is realistic."
Ask: "How would these results change your practice's financial health?" Mention your team's years of experience as a quiet trust signal rather than a boast.


"Mention your team's years of experience as a quiet trust signal rather than a boast."
Dig deeper to uncover real concerns
The first objection is not always the root issue. Ask what makes switching hard. Explore transition risks, reporting needs, or training time.
Clarify which outcomes matter most, such as cleaner claims, faster reimbursement, or better visibility on aging. Use specific examples to show how your process reduces friction and keeps the revenue cycle moving.
4. Quantify your ROI to demonstrate value
Present clear financial data to show why your work delivers results. Highlight metrics that matter: track higher collection rates, reduced claim errors, and faster reimbursements.
Add rates for denials, time-to-follow-up on medical claims, and simple revenue cycle management (RCM) analytics that show where cash gets stuck. Bring short case studies and easy visuals so leaders can see the impact at a glance.
Break down the costs of in-house billing: compare salaries, software fees, taxes, training, and turnover with the net gains from billing outsourcing. Convert improvements into monthly dollars and a payback timeline. Tie the story to daily practice management so decision makers understand the changes between week one and month one.
For a quick overview of tools that support this analysis, see Tebra's billing software for billing companies.
5. Close deals with a strong follow-up strategy
Use a clear closing line that invites action, then set the next step on the calendar. Confirm who owns the task, what will be delivered, and when you'll check back in. Treat follow-up as part of the value you provide, not an afterthought.
Research shows that many decisions take several touches. Plan a steady cadence that mixes a brief phone call with concise email marketing updates. Each touch should add something useful, such as a new stat, a short case study, or a reference from a similar practice.
Keep simple CRM hygiene. Log notes, set the next action date, track status, and avoid duplicates so your sales team stays aligned. Consistent follow-up builds trust and shortens the path to a yes.


"Consistent follow-up builds trust and shortens the path to a yes."
6. Maintain client relationships beyond the sale
Keep clients engaged and show you're invested in their long-term success. Tie check-ins to goals that matter in practice management, such as fewer bottlenecks and faster hand-offs in healthcare billing.
- Check in regularly: Schedule brief reviews to surface wins, risks, and next steps. Share simple progress notes and agree on one action to complete before the next meeting. Small, steady updates build trust.
- Ask for referrals: Use a structured request at milestones. When a target is met, ask for referrals and make it easy with a short blurb they can forward. Track who referred whom so you can thank them.
- Share proof: With permission, publish short case studies and gather concise testimonials. Highlight the problem, the fix, and the result in plain language. Then send the client a copy so they can share it with their network.
7. Justify cost increases when the time is right
Lead with measurable outcomes. Review financial performance with the client and show how your work improved collections, shortened time to reimbursement, and drove faster payments. Use simple reports that compare baseline results with current metrics so the value is easy to see.
Explain cost drivers with care. Note the staffing mix, including a full-time medical billing specialist dedicated to their account and the ongoing credentialing work required to keep payer enrollments current.
Tie each cost to a concrete benefit, such as fewer errors, cleaner claims, and quicker issue resolution. Close by proposing a reasonable adjustment, the effective date, and the specific service improvements they can expect.


"Lead with measurable outcomes."
Connect sales to RCM and compliance signals
Strong promises land when they map to day-to-day operations. Show clean medical coding and correct CPT usage, and link to the CPT coding overview to explain why standardized procedure codes reduce rework. Confirm credentialing timelines and payer enrollments to lower onboarding risk for Medicare and commercial reimbursement.
Tie outcomes to RCM metrics. Explain how you prevent denials, shorten follow-up on medical claims, and improve time to payment. For hospital-affiliated groups, reference the 3-day payment window so teams understand how pre-admission services may be bundled under Medicare rules.
Where diagnosis accuracy matters, point teams to the ICD-10-CM guidelines. Keep exhibits short and the numbers easy to verify so practices see what changes next week and next month.

Sell your services more effectively
Adopting a sales mindset means understanding each practice's needs and showing measurable outcomes. When you define an ideal client, refine your pitch, handle objections, and follow through, you build trust that lasts. The payoff is stronger revenue cycle management, steadier cash flow for medical practices, and sustainable growth for medical billing services.
If you want technology that supports that work, Tebra's EHR+ unites clinical and financial tools. Explore our EHR software, then see how billing for billing companies helps with reporting, claims, and collections. Share the resources with your team and choose the next step that fits your goals.
FAQs
FAQ about medical billing sales
You might also be interested in
Learn the secrets of high-performance medical billing companies in our medical billing benchmark report.
- Current Version – Nov 18, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.





