
-
- Capture encounter type and modality consistently so telehealth services map to accurate telehealth billing and smoother reimbursement.
-
- Verify the payer before each visit to confirm coverage, required documentation, and submission rules that keep payments on track.
-
- Review policies and workflows regularly so telehealth billing stays current, and reimbursement remains predictable across every payer.
-
- Medicare’s pandemic-era flexibilities lapsed on October 1, 2025, and CMS placed a short claims hold, so verify coverage details now to avoid denials once payments resume.
Delivering care via telehealth is an important part of keeping up with innovation and patient demand for many private practices. With the right telehealth platform, seeing patients via synchronous video is both easy and efficient. But the requirements and regulations surrounding telehealth billing can be anything but.
This guide brings together must-have references for telehealth services and telemedicine. You will find plain-language steps on codes, modifiers, and place of service rules, plus what to verify with each payer. We also note 2025 updates that affect providers, reimbursement, and coverage across healthcare programs so teams can confirm current policy before submitting claims.
How telehealth billing works

There are 6 steps to proper telehealth billing:
- Start with documentation: Record what occurred during the encounter, who was present, and the type of communication technology used.
- Select the correct codes: Choose CPT or HCPCS codes based on the service delivered. CPT is standard for most professional services, while HCPCS may be required by some payers.
- Include the right place-of-service: Match the place-of-service code to the technology used and payer requirements — especially for audio-only or asynchronous care.
- Submit the claim: Once properly coded, file the claim with supporting documentation to reflect medical necessity and care provided.
- Track payment or denials: Monitor claim status and address any issues quickly to prevent delays in reimbursement.
- Verify coverage rules: Always confirm whether the service and technology used are covered by Medicare or commercial payers before billing. If you are unsure about coverage, check the Medicare telehealth services guidance and your commercial payer policies before filing the claim.
2025 policy snapshot: Medicare and Medicaid
For Medicare, CMS maintains Medicare telehealth services under the annual physician fee schedule. Key 2025 updates flow through the final rule, which sets coverage and payment mechanics for virtual care and clarifies items that remained after the public health emergency (PHE) waiver period. Verify current allowances before you bill.
For Medicaid, states administer Medicaid services and benefits, so coverage varies. Check state rules, especially for managed care arrangements, and confirm plan specifics for Medicare Advantage when patients are enrolled there instead of Original Medicare. Start with the federal overview, then confirm state and plan details.
Before filing, confirm any state updates and plan bulletins. When double-checking coverage and payment language, favor official .gov sources.
October 1, 2025, update: Key flexibilities have expired
Congress did not pass a continuing resolution by September 30, so several Medicare telehealth flexibilities expired on October 1, 2025. CMS issued an MLN notice directing MACs to place a temporary claims hold (about 10 business days) to avoid mass reprocessing if Congress restores coverage.
You can submit claims, but payment is held until that pause lifts. Expect tighter rules on originating site (home generally no longer eligible), geographic limits, narrower audio-only coverage, and changes for FQHC/RHC distant-site billing, with behavioral health exceptions. Verify plan bulletins before scheduling.
Here's what to verify now:
- Whether the patient's home still qualifies for the service you plan to bill, and which facility settings remain eligible originating sites.
- If audio-only is still payable for your scenario and what documentation is required.
- Whether your clinician type remains eligible, and the current FQHC/RHC rules.
- Any MA/Medicaid plan variations compared with traditional Medicare.
Understand service locations
Rules distinguish the originating site from the distant site, and many policies recognize the patient's home. Some also include a nursing facility. Billing can differ in inpatient and outpatient settings, so match codes and documentation to the setting you used.
Know your clinic type
FQHC sites (federally qualified health centers) and RHCs (rural health clinics) often have specific flexibilities and payment methods. Review your state's telehealth policy and plan contracts each year to confirm what applies to your teams.
Codes, modifiers, and documentation essentials
Pick codes that reflect the service delivered and the technology used. Start simple. Map the visit type, then confirm payer rules before you submit:
- Codes: Most telehealth evaluation and management office visit services use CPT codes (current procedural terminology) maintained by the AMA. Some virtual services require HCPCS codes instead. Match code selection to what happened in the encounter.
- Modifiers: Add a modifier when the payer requires it for telehealth. Use the modifier listed in the plan policy for the service you performed.
- Place of service: Report the correct POS code based on payer guidance. Review the place of service codes to reflect where the patient received care and where the clinician was located.
- Eligibility and roles: Confirm that the billing site provider type is eligible to submit claims for the selected codes. Verify patient eligibility before the visit.
- Documentation: Note the clinical elements and the technology. Include history, exam when required, medical decision making, and the modality used.
- Payer variations: Plans may differ on code lists, documentation, and required modifiers. Check policy updates each year and after major rule changes.
Disclaimer: Policies vary by payer. Always confirm code lists, POS code use, and modifier requirements with the plan before filing the claim.
Reimbursement by payer type (fee-for-service and managed care)
Reimbursement follows the contract you bill against. In fee-for-service, the payer pays for each covered unit once a clean claim is on file. In managed care, including Medicare Advantage, plans apply federal baselines and their own coverage criteria. Check plan materials before the visit so there are no surprises.
Coverage depends on who can bill and who is enrolled. Eligible clinicians and the beneficiary's plan status determine whether telemedicine services and other health services are payable. Medicare sets the starting point for virtual care. State rules and commercial policies layer on top. For state-by-state lookups, review the CCHP state telehealth policies and confirm details with each plan.
Here's a quick checklist:
- Verify eligibility: Confirm the patient's plan, virtual-care coverage, and cost-sharing before scheduling.
- Confirm codes and fields: Check covered CPT/HCPCS, required modifiers, and the correct POS entry for the plan.
- Confirm documentation: Ensure notes support medical necessity and reflect the modality used for the visit.
Staying strict on eligibility, code selection, and documentation reduces rework and keeps reimbursement predictable across fee-for-service and managed care.
Special services and scenarios
Some services and settings have extra rules. Review what is covered, who can deliver it, and what documentation each plan expects.
- Behavioral health and mental health often allow broader virtual care. Many payers cover telemedicine services using a video telecommunications system and sometimes by phone. Confirm audio allowances, any in-person follow-up, and supervision rules before you schedule.
- Remote patient monitoring (RPM) is billed differently from a standard visit. These management services rely on device data and time-based work rather than a single encounter. Check code requirements and note how your payer wants readings, time, and contact documented.
- Care setting affects coverage and payment. Inpatient policies are not the same as outpatient rules. A nursing facility may have its own terms. Match codes, place of service, and notes to the setting are recorded in the chart.
- Modality matters for payment. Real-time video is often treated like a face-to-face visit. Asynchronous tools handle images, messages, and data review. Record the technology used and verify that the plan covers that modality for the service you provided.
- For telemental health, the in-person requirement tied to home-based services now applies post-October 1, 2025, with limited exceptions. Watch for CMS clarifications.
Coverage lists can change. So, recheck your plan guidance for telemedicine services when you add a new program, expand a setting, or update workflows.
Documentation and claim-filing checklist
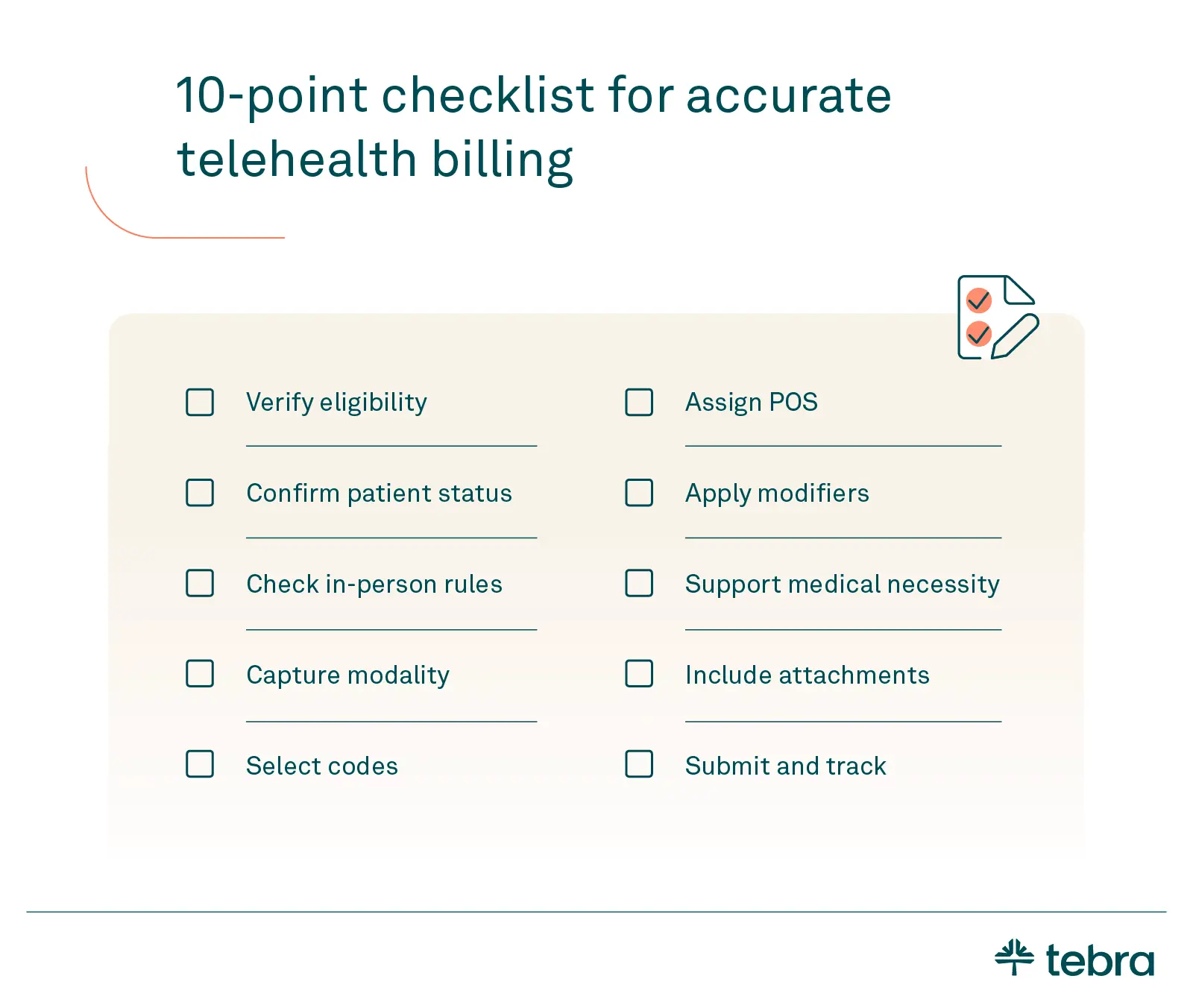
Use this quick checklist to standardize records for virtual care. It helps teams capture what payers expect, avoid preventable edits, and keep claims moving. Complete these steps before and after the visit to support clean telehealth billing.
- Verify eligibility: Confirm the plan, virtual-care coverage, and cost sharing with the payer before telehealth visits.
- Confirm patient status: Note whether the patient is an established patient when the plan requires it for specific services.
- Check in-person rules: Identify any in-person or prior in-person visit requirements and record timelines in the chart.
- Capture modality: Document the technology used and whether the visit was audio-video or audio-only.
- Select codes: Choose CPT/HCPCS codes allowed under plan telehealth billing and match codes to what was performed.
- Assign POS: Enter the appropriate POS code for the patient location and clinician site per plan guidance.
- Apply modifiers: Add the required modifier for telehealth when the plan lists one.
- Support medical necessity: Record history, exam when required, and medical decision-making that aligns with the service billed.
- Include attachments: Add payer forms, consents, or device readings if the plan asks for them.
- Submit and track: File the claim, watch for responses, and correct denials with updated fields or notes.

Putting it into practice
Clean telehealth billing and virtual care start with consistent documentation. Confirm the codes, the modifier, and the POS code before you submit. Verify payer rules for coverage and cost sharing so reimbursement stays predictable. Keep notes clear about the modality and the service delivered, especially for telemedicine services.
Teams of providers and every healthcare professional involved should review policies on a set cadence and update checklists as rules change. If you want tools that help standardize coding and claims workflows, check out the Tebra EHR software. For more guides and insights across private practice operations like this one, explore our resources on Tebra's resource and knowledge base.
Telehealth resources for private practices
When a coding question pops up or a plan wants a citation, start here. These resources are reliable, kept current, and easy to navigate. Bookmark the CMS hub for national rules, use CCHP for state changes, and lean on AMA guidance for day-to-day questions. Whenever possible, rely on official gov pages.
- AMA (American Medical Association) quick guide to telehealth: Overview of services, implementation, coding, and payment.
- Medicare telehealth services: Federal hub for coverage and the current code lists.
- CY 2025 physician fee schedule fact sheet: Annual updates that shape virtual-care payment.
- State telehealth policies: Search state-by-state laws and reimbursement rules.
- Medicaid telehealth: Federal overview with links to state program details.
- Telehealth policy cliff (NCTRC): Plain-English tracker of October 1 changes and contingency planning checklists.
If a plan requires specifics beyond these, review its policy manual and any plan FAQ pages before scheduling or submitting claims.
FAQs
FAQs about telehealth billing for medical practices
You might also be interested in
How patients find and pick their doctors. We surveyed more than 3,900 patients nationwide to understand factors that influence how they choose a doctor and why they keep coming back. Download the free report.
- Current Version – Oct 28, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.





