Overview
-
- 67% of patients are concerned that the bill will impact their access to care, medications, or vaccines.
-
- 40% of patients think the bill puts them more at risk of medical debt or bankruptcy.
-
- 61% of Americans say the bill has decreased their trust in the US healthcare system.
-
- Nearly 7 out of 10 medical care providers (68%) say the bill harms vulnerable patients.
The One Big Beautiful Bill has officially become law, but are Americans ready for what it means in practice? Tebra surveyed patients and healthcare providers across the United States to understand how this sweeping legislation is landing in real-world care settings.
Many patients are unclear on core provisions like Medicaid cuts, work requirements, and eligibility changes, and are unsure whether they'll still have access to critical care like vaccines. At the same time, providers are divided on whether the law will reduce red tape or introduce new burdens. Across both groups, many are already reporting rising confusion, fear, and mistrust in the US healthcare system.
Key takeaways
- 67% of patients are concerned that the bill will impact their access to care, medications, or vaccines.
- 40% of patients think the bill puts them more at risk of medical debt or bankruptcy.
- 61% of Americans say the bill has decreased their trust in the US healthcare system.
- Nearly 7 out of 10 medical care providers (68%) say the bill harms vulnerable patients.
Confusion around eligibility, work requirements and coverage transitions can trigger delayed care, missed vaccinations and higher out-of-pocket exposure.
A law few understand, but many patients will feel
Plan-language outreach, upfront benefit checks at scheduling and proactive price transparency help maintain continuity and reduce fear-driven avoidance.
Most patients have heard of the One Big Beautiful Bill, but few fully understand what it includes or how it may affect their care. As the legislation takes effect, concern is growing among Americans about its real-world implications.
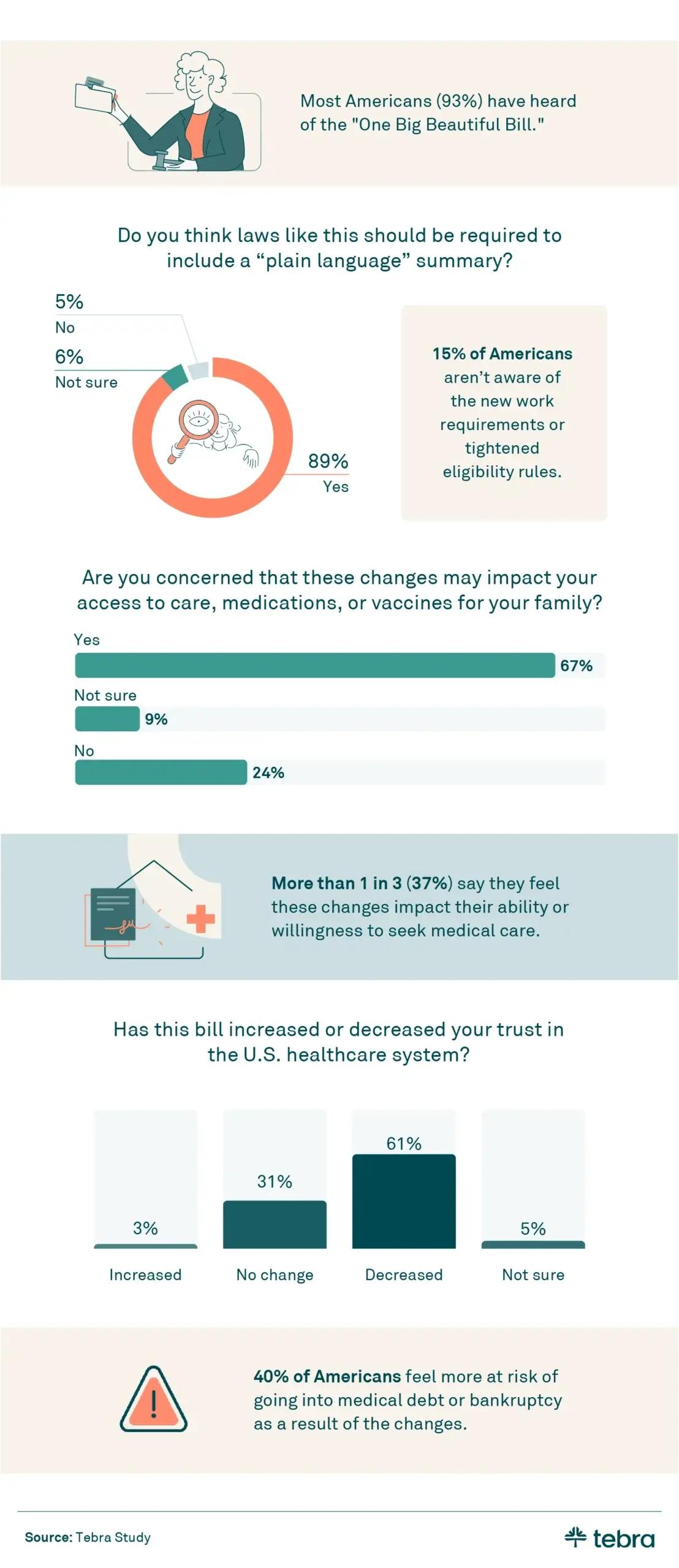
- 67% of patients are concerned that the bill will impact their access to care, medications, or vaccines.
- More than 1 in 10 Americans (15%) aren't aware of the One Big Beautiful Bill's new work requirement, which mandates that many Medicaid recipients must prove they are employed, actively seeking work, or enrolled in job training programs in order to keep their health coverage.
- Over 1 in 3 (37%) say the bill has impacted their ability or willingness to seek medical care.
- 40% of Americans say they feel more at risk for medical debt or bankruptcy as a result of the bill.
- 3 in 5 Americans say the bill has decreased their trust in the US healthcare system
These responses point to rising fear and confusion among patients, especially those navigating complex or changing insurance coverage. Private practices can play a key role in bridging the gap by offering transparent communication, clarifying eligibility requirements, and ensuring that patients feel supported as they navigate new challenges in access and affordability.
For practices, policy complexity often shows up as more forms, denials, and follow-ups — lengthening revenue cycles and intensifying burnout.
Paging Dr. Red Tape: What providers think
Integrated EHR + billing, templated documentation, and automation for routine eligibility/authorization tasks can absorb new compliance load and keep clinical time focused on care.
The One Big Beautiful Bill may promise simplification, but many healthcare providers say it's already making day-to-day care more complicated. From rising administrative tasks to concerns for vulnerable patients, providers are feeling the strain.
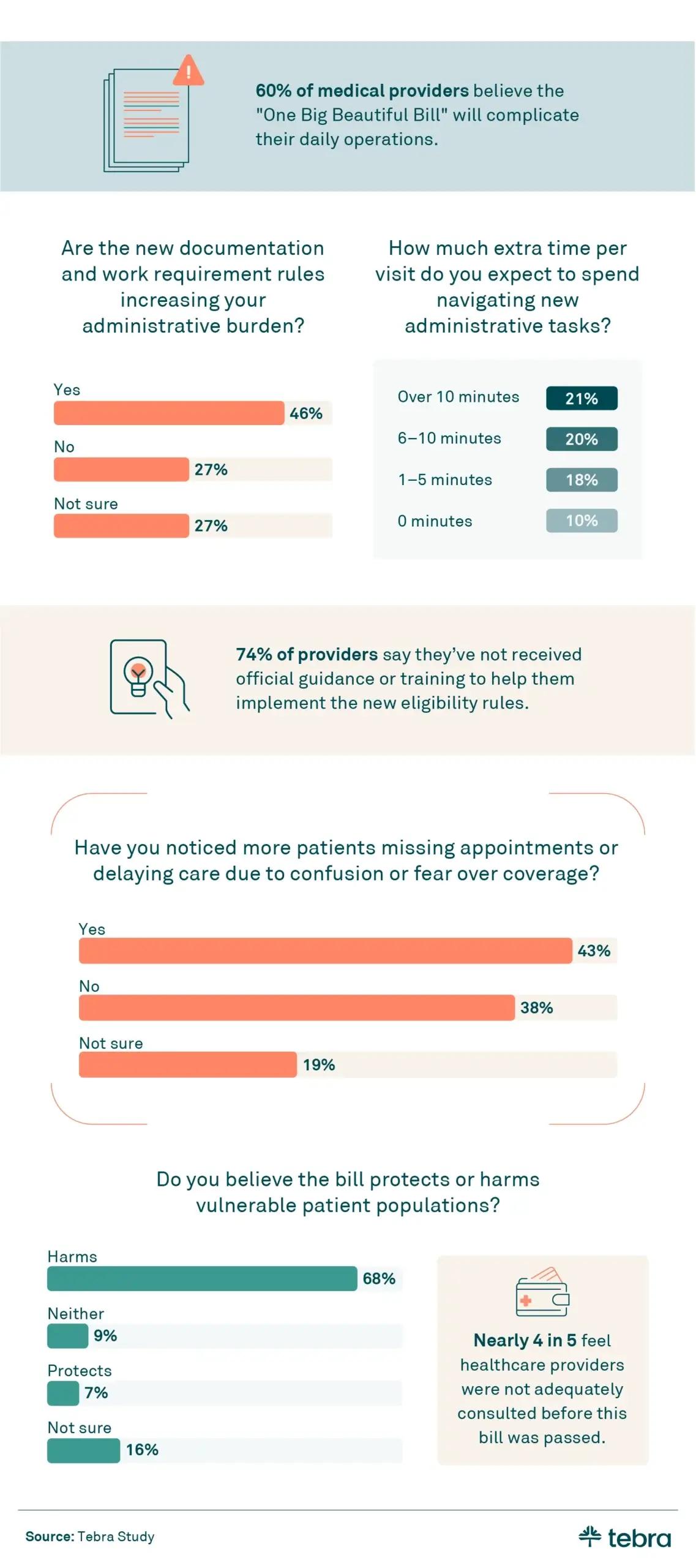
- Nearly 4 in 5 feel healthcare providers were not adequately consulted before this bill was passed.
- 68% of medical care providers believe the bill harms vulnerable patients.
- 46% say the bill's new documentation and work requirement rules are increasing their administrative burden.
- 43% have noticed more patients missing or delaying appointments due to confusion or fear over coverage.
To manage the growing complexity, private practices need systems that work with them, not against them. An all-in-one EHR can help reduce the burden of new documentation rules, streamline communication, and keep practices running smoothly. By automating routine tasks and simplifying patient outreach, providers can focus more on care and less on red tape.
In shifting policy environments, playbooks that standardize communication and access tend to outperform ad-hoc fixes.
How private practices can move forward with clarity and care
Codify scripts for staff, automate reminders and eligibility checks, and centralize messaging in patient portals to reduce no-shows and preserve patient trust.
As the One Big Beautiful Bill takes hold, both patients and providers are bracing for change, and some of it is already in motion. Patients worry about coverage, access, and cost. Providers feel the weight of unclear rules, rising paperwork, and reduced trust in the system.
For private practices, this moment is both a challenge and an opportunity. Practices can set themselves apart by offering reliable communication, compassionate support, and the tools patients need to stay engaged in their care. Internally, reducing the impact of administrative demands is key to maintaining provider well-being and practice efficiency.
Solutions like Tebra EHR+ give practices an edge by combining clinical, billing, and patient communication tools in one platform. With built-in automation and transparent pricing, practices can adapt more easily to policy changes and help patients do the same. Amid uncertainty, consistency and clarity go a long way.
Methodology
Tebra surveyed 436 providers, ages 22–73; 31% were men, 68% women, and 2% identified as non-binary. Thirty-five percent worked in a hospital setting, 27% in private practice, 14% in community health centers, 3% in academic research, 2% in pharmacies, 1% in urgent care, and 19% in other unspecified settings.
Tebra also surveyed 523 patients, ages 18–81; 49% were men, and 51% were women. Fifty-nine percent had private insurance, 19% were insured through Medicaid, 13% were uninsured, 8% were insured through Medicare, and 1% were not sure about their current healthcare coverage. Percentages in this study may not equal 100 due to rounding.
About Tebra
Tebra, headquartered in Southern California, empowers independent healthcare practices with cutting-edge AI and automation to drive growth, streamline care, and boost efficiency. Our all-in-one EHR and billing platform delivers everything you need to attract and engage your patients, including online scheduling, reputation management, and digital communications.
Inspired by "vertebrae," our name embodies our mission to be the backbone of healthcare success. With over 165,000 providers and 190 million patient records, Tebra is redefining healthcare through innovation and a commitment to customer success. We're not just optimizing operations — we're ensuring private practices thrive.
Fair use statement
This content may be shared for noncommercial purposes with proper attribution. Please include a link back to Tebra when referencing or quoting this article.






