
- 3 in 10 providers say 26–50% of their care is prevention-focused.
- 3 in 10 providers say they have prescribed medication when a lifestyle change would have been more effective.
- Nutrition guidance is the most frequently recommended lifestyle intervention and the topic that providers feel most confident discussing with patients.
- Just 7% of providers feel confident in their ability to counsel patients on substance abuse.
- 1 in 4 providers feel pressure to integrate preventive care into their practices.
Preventive care, which focuses on identifying risks early and supporting lifestyle changes before conditions worsen, is becoming a larger part of everyday healthcare. As more patients seek guidance on nutrition, activity, stress, and other lifestyle factors, providers are working to integrate these prevention-first approaches into routine care.
Tebra surveyed medical providers to better understand how they are delivering preventive care today and where they still feel gaps in training, confidence, and systemic support.
Prevention is gaining ground, but confidence gaps remain
As patients seek proactive care options, providers are adapting via lifestyle-focused interventions and preventive screenings. However, confidence varies by clinical topic and social determinants of health.
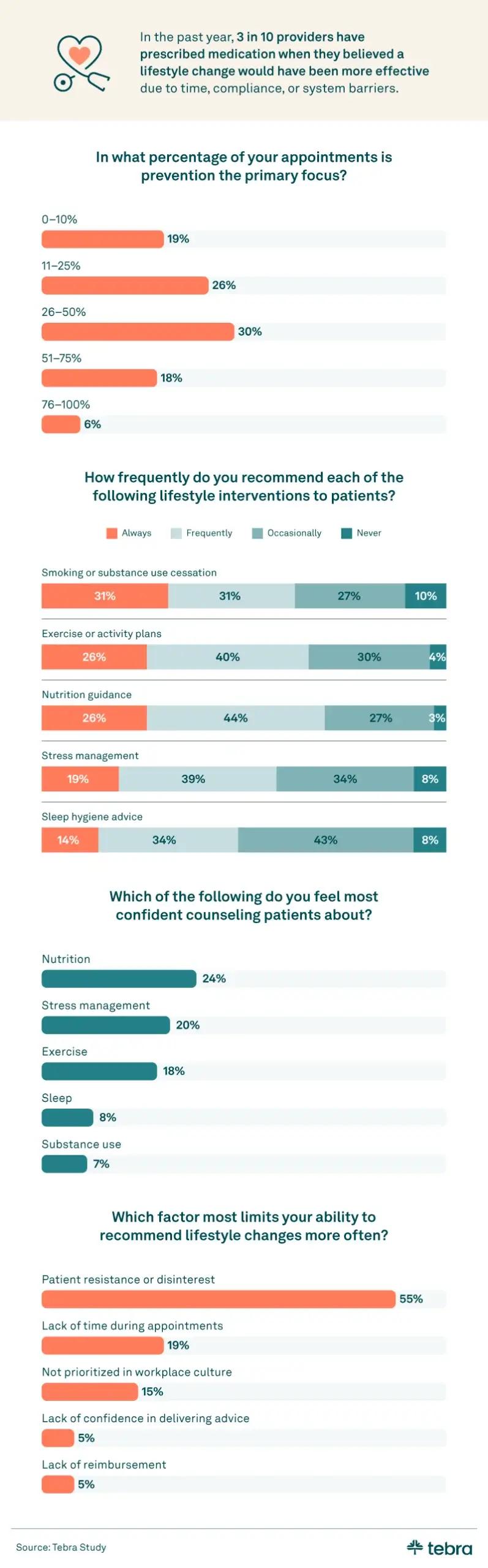
Three in 10 providers reported that 26–50% of their care is now focused on prevention. This signals a meaningful shift toward wellness-first care models, though not yet a majority. Among preventive approaches, nutrition guidance was the most common and confidently delivered recommendation, with 24% of providers citing it as their strongest area.
However, provider confidence sharply declines in more complex or sensitive areas. Nearly 1 in 3 providers (29%) expressed doubt in their ability to counsel patients on substance abuse, and just 7% said they felt confident doing so. These disparities may impact how consistently patients receive preventive guidance, especially for conditions that require behavioral or psychosocial support.
To build confidence across prevention topics, providers can seek out targeted training in areas like motivational interviewing, behavioral health, or trauma-informed care. Creating a referral network of specialists for sensitive issues can also ensure patients get comprehensive support while keeping care coordinated within the practice.
Payment and training models shape provider priorities
The structure of healthcare, including reimbursement CPT codes and value-based care models, directly influences how often providers can focus on prevention.

Nearly 2 in 5 providers (39%) said their organization uses a value-based care model. In this model, providers are rewarded based on patient outcomes rather than the volume of services delivered. Among those working within value-based systems, 36% said their focus on lifestyle and prevention increased.
When asked what would help them provide more prevention-focused care:
- 33% of providers said more training would make the biggest difference
- 22% said they needed more appointment time dedicated to preventive care
Billing codes also played a key role. Nearly half of all providers (49%) said current billing codes do not adequately support lifestyle counseling and prevention. Only 18% said they do, and 34% were unsure.
Private practices looking to expand preventive care can start by exploring continuing education options that focus on lifestyle medicine and patient engagement. Involving clinical and administrative staff in conversations about appointment scheduling and billing workflows may also help identify opportunities to carve out time for prevention. Leaning into EHR tools that support patient education, follow-up reminders, and documentation shortcuts can streamline the process and make preventive care a more natural part of every visit.
Providers use a mix of formal and informal tools to support prevention
Many providers lack formal training in prevention-focused care, supplementing their knowledge through continuing medical education (CME) and informal peer-led resources.

About 1 in 4 providers (24%) said they have not received any formal training in prevention or lifestyle medicine. To stay up to date on prevention or lifestyle medical practices, most providers (75%) relied on continuing medical education (CME). Yet, 32% said they use medical podcasts to stay informed, and 27% have relied on social media. Altogether, more than half (54%) reported using nonclinical resources to learn about prevention-focused care.
While these tools can be helpful, they are not a substitute for comprehensive, evidence-based training. Nearly half of all providers (49%) said they would feel more confident delivering prevention-first care if they had access to more CME or structured training programs. Another 49% wanted better educational materials to share with patients, 44% said they needed more time during appointments, and 39% wanted approved EHR templates to support lifestyle counseling.
To build skills and confidence, providers can explore CME opportunities focused on lifestyle medicine, patient communication, and behavior change. Practices may also consider integrating ready-to-use patient handouts or digital resources into their EHR system to support consistent, time-efficient prevention conversations.
A shift worth supporting
As prevention becomes a more prominent part of patient care, providers are navigating new responsibilities, pressures, and opportunities. Many feel energized by the shift toward wellness-focused treatment, but still lack the training and systemic support to confidently deliver it.
By investing in education and leveraging existing billing pathways, private practices can be part of this growing movement toward proactive care. When providers feel prepared and empowered, patients benefit from more holistic treatment and healthier futures.
Methodology
Tebra surveyed 289 medical providers who deliver direct care to patients with chronic or lifestyle-related conditions such as diabetes, hypertension, and heart disease. Participants worked across a variety of healthcare settings, including hospitals (51%), private practices (19%), community health clinics (15%), academic medical centers (6%), and telehealth-only practices (1%).
Most respondents identified as women (71%), followed by men (28%) and nonbinary individuals (1%). The sample included registered nurses (63%), physicians (16%), nurse practitioners (8%), allied health professionals (7%), and physician assistants (6%). Respondents worked within nonprofit health organizations (38%), for-profit private providers (36%), government or public health systems (23%), and as independent contractors or solo providers (3%).
About Tebra
Tebra, headquartered in Southern California, empowers independent healthcare practices with cutting-edge AI and automation to drive growth, streamline care, and boost efficiency. Our all-in-one EHR and billing platform delivers everything you need to attract and engage your patients, including online scheduling, reputation management, and digital communications.
Inspired by "vertebrae," our name embodies our mission to be the backbone of healthcare success. With over 165,000 providers and 190 million patient records, Tebra is redefining healthcare through innovation and a commitment to customer success. We're not just optimizing operations — we're ensuring private practices thrive.
Fair use statement
This article’s findings may be shared for noncommercial purposes with proper attribution. If you reference or republish any content, please include a link back to Tebra.





