
- 67% of people schedule end-of-year visits to beat their deductible reset (15% every year; 52% some years)
- 16% book non-urgent visits to use flexible spending accounts (FSA) funds before they expire
- 27% delay needed care until later in the year once their deductible is met.
- More than 1 in 10 patients (11%) say deductibles often dictate their medical decisions.
- 82% of healthcare professionals see a spike in appointments in December, and 67% feel more burned out in December than in any other month.
- 57% of healthcare professionals have missed major holidays due to patient demand. This year, 1 in 5 will miss Thanksgiving, and 1 in 4 will miss either Christmas Eve or Christmas Day.
As the calendar winds down, the healthcare system faces one of its busiest and most challenging periods. A Tebra survey of 750 Americans and 250 healthcare professionals reveals how the end-of-year push to use up benefits and meet deductibles creates a perfect storm for patients and providers alike.
For patients, it's a rush to maximize insurance coverage and avoid wasting funds set aside for healthcare purposes only. For healthcare workers, it's a season marked by longer hours, missed holidays, and mounting burnout. Understanding this annual surge sheds light on how insurance structures drive behavior and what it means for private practices across the United States.
End-of-year rush for healthcare appointments
Many patients prioritize insurance deadlines over clinical urgency, producing a predictable December spike in appointments as people try to maximize coverage or use expiring benefits.
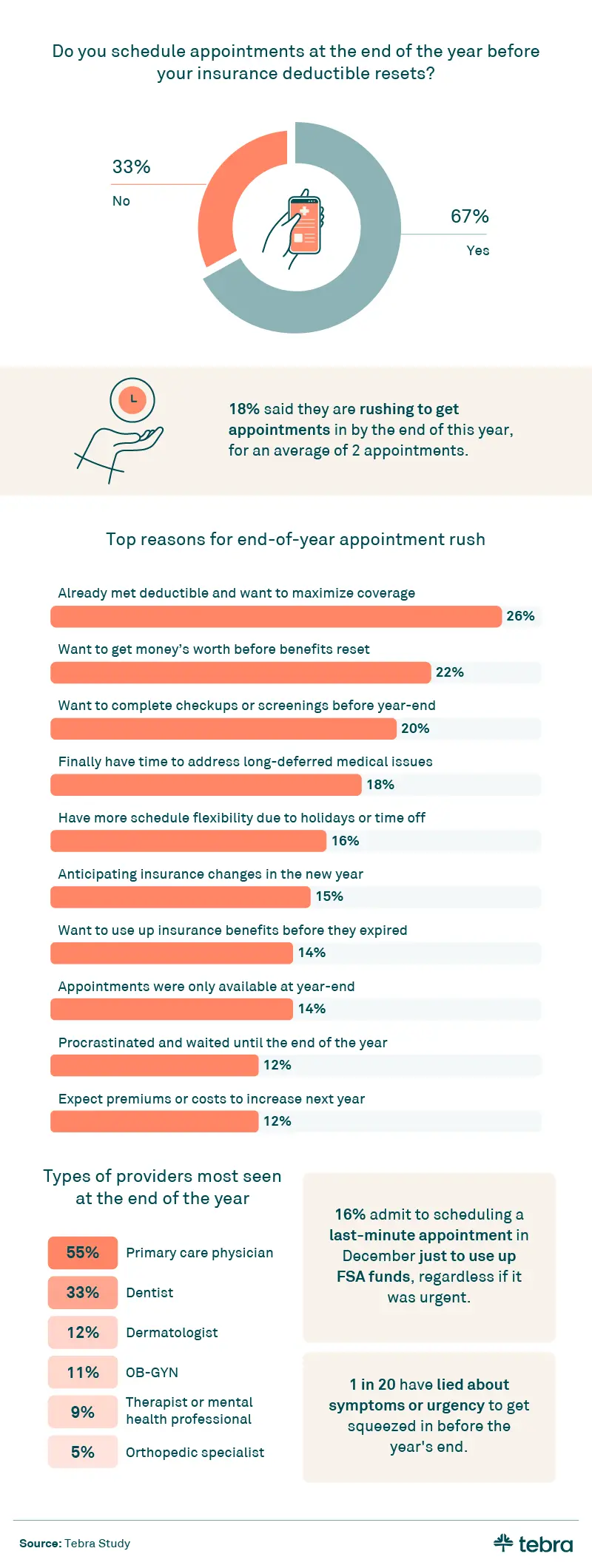
A majority of patients (67%) reported scheduling medical visits toward the end of the year to avoid the resetting of their deductible. For some, this is an annual ritual: 15% said they make these appointments every year, and 22% admitted feeling pressure to "get their money's worth" from their insurance.
The financial motivation doesn't stop at deductibles. About 16% of patients book non-urgent appointments just to use up FSA funds before they expire. This urgency to avoid waste can lead to overbooking or unnecessary visits.
That demand comes at a cost. More than 1 in 4 patients (27%) have accepted inconvenient or undesirable appointment times to be seen before the year ends. In some cases, urgency trumps honesty: 5% of patients admitted exaggerate symptoms to secure last-minute slots.
- Private practice takeaway: Start outreach in mid-November with reminders about deductible resets and FSA deadlines.
- Publish clear “last appointment” windows and offer telehealth alternatives.
- Reserve daily last-minute slots and route them to a rotating on-call clinician to avoid overtime.
- Automate reminders (SMS + email) and add an online “year-end booking” banner to capture demand without staff lift.
- Offer an end-of-year benefits checklist or short financial counseling link to reduce unnecessary visits.
Deductible rules lead to delayed care and questionable spending
Insurance plan design not only shifts when people seek care — it can change whether they seek it at all and encourage spending solely to avoid losing benefits.
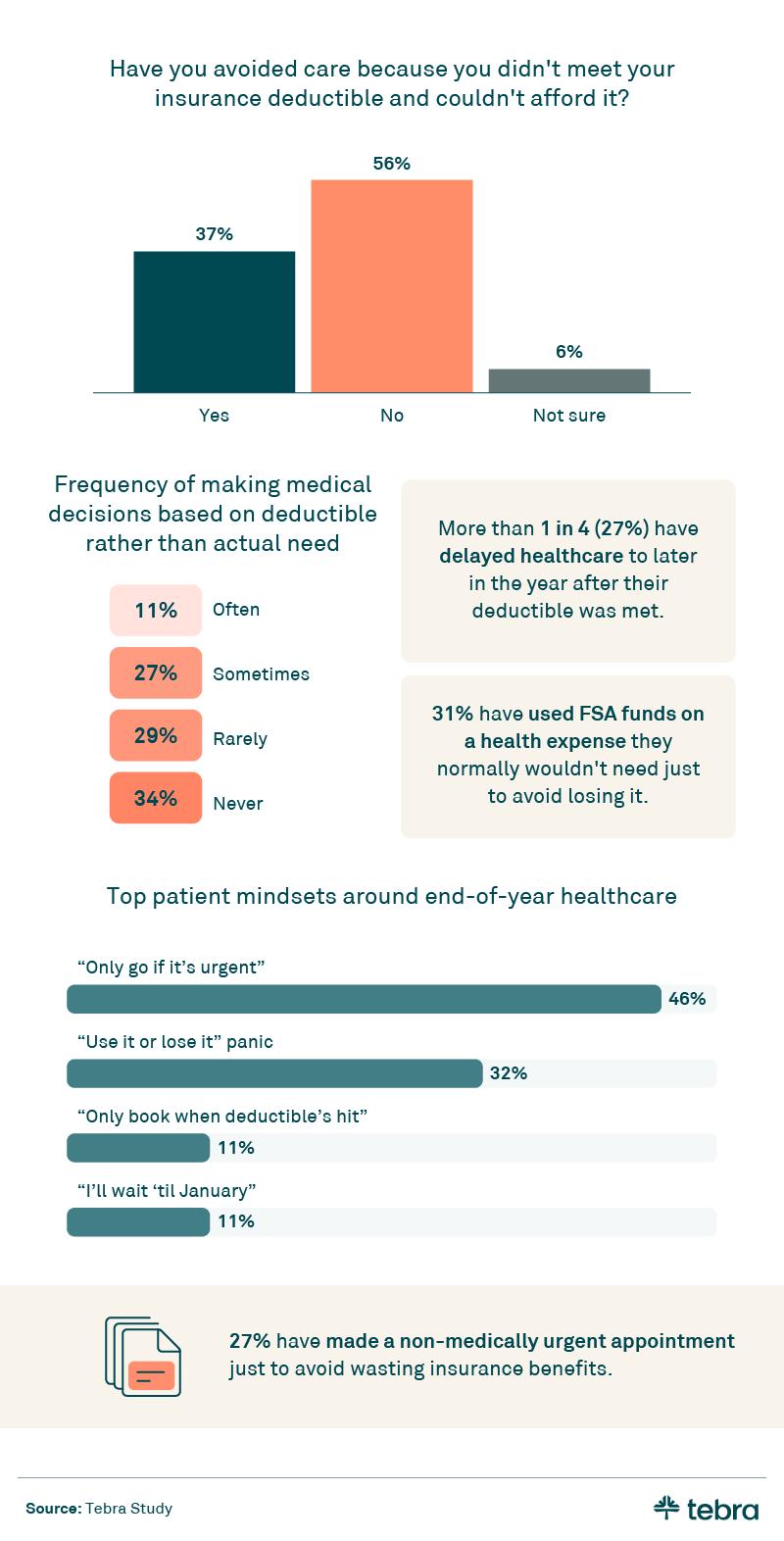
More than 1 in 10 insured Americans (11%) said they often make medical decisions based on their deductible rather than actual need. This includes delaying care or making questionable purchases to use up funds.
In fact, 27% of patients said they've intentionally delayed a needed appointment until later in the year, once their deductible was already met. Another 27% scheduled appointments for non-urgent issues simply to avoid wasting benefits.
Even spending habits are shaped by the end-of-year deadline. Thirty-one percent of patients admitted to using their FSA funds on items or services they didn't truly need so they wouldn't lose the money.
Advice for private practices: Educate patients year-round about how and when to use their benefits wisely. Use digital communication tools, like email campaigns, SMS reminders, or intake forms, to guide patients toward timely, medically appropriate care. Offering financial counseling or providing a benefits checklist at midyear can also help prevent the year-end scramble and support better health outcomes.
Healthcare workers feel the weight of the year-end surge
While patients focus on benefits, healthcare professionals face a different reality: longer hours, missed holidays, and rising burnout.

Among healthcare professionals surveyed, 82% reported a clear spike in appointments during December. This is likely one major reason why 67% said they feel more burned out in December than any other month of the year.
The rush also impacts personal lives. Nearly 3 in 5 providers (57%) have missed holiday celebrations due to the year-end surge, including 34% who missed Thanksgiving and 25% who missed Christmas. Seventeen percent missed holiday travel altogether. This year, 1 in 5 expect they'll miss Thanksgiving, while 1 in 4 said they won't be home on either Christmas Eve or Christmas Day.
This pressure is reshaping how some providers view the healthcare system. Nearly three-quarters (74%) said they believe current insurance structures create unnecessary urgency or poor timing for patient care. The same percentage have worked extended hours just to keep up with the December demand. Alarmingly, 1 in 4 have considered leaving the healthcare field altogether because of the stress tied to year-end workloads.
How practices should prepare for the end-of-year appointment surge
The year-end healthcare rush is a reflection of how insurance structures influence patient decisions and strain provider capacity. From delayed care and unnecessary spending to staff burnout and missed holidays, the impact is widespread.
For private practices, anticipating this annual demand is critical. Thoughtful scheduling, expanded hours, and transparent communication with patients can help manage expectations and reduce strain. Long-term, rethinking how benefit structures affect care timing could lead to better outcomes for patients and providers alike.
Methodology
Tebra surveyed 750 Americans and 250 healthcare professionals, including physicians, nurses, and front office staff, to understand how end-of-year health insurance deadlines influence patient behavior and impact providers.
About Tebra
Tebra, headquartered in Southern California, empowers independent healthcare practices with cutting-edge AI and automation to drive growth, streamline care, and boost efficiency. Our all-in-one EHR and billing platform delivers everything you need to attract and engage your patients, including online scheduling, reputation management, and digital communications.
Inspired by "vertebrae," our name embodies our mission to be the backbone of healthcare success. With over 165,000 providers and 190 million patient records, Tebra is redefining healthcare through innovation and a commitment to customer success. We're not just optimizing operations — we're ensuring private practices thrive.
Fair use statement
If you'd like to share these insights, you're welcome to do so for noncommercial purposes. Please link back to Tebra and provide proper attribution.





