
- 69% of Americans have been surprised by the final cost of a routine medical service, even after checking insurance or asking about pricing in advance.
- Nearly 1 in 3 Americans (32%) didn’t understand the charges on their last medical bill.
- 47% of Americans have avoided care in the past 12 months after receiving a medical bill that was higher than expected.
- 60% of Americans expect to delay or skip at least one type of medical care in 2026 due to cost concerns.
For many Americans, understanding what healthcare actually costs feels like a gamble. Patients do their best to prepare — checking insurance coverage, asking about pricing — but still sometimes walk away with bills far higher than expected.
In a recent survey of over 1,000 Americans, Tebra uncovered just how common these billing surprises are and how they're affecting patient care decisions. As unexpected costs and confusing charges chip away at patient trust, private practices have an opportunity to rebuild it through transparency, education, and better communication.
The routine care price gap
Even routine medical care can come with a price tag that catches patients off guard, often due to a lack of upfront price transparency. Despite efforts to anticipate costs, many Americans find themselves surprised when the final bill arrives.
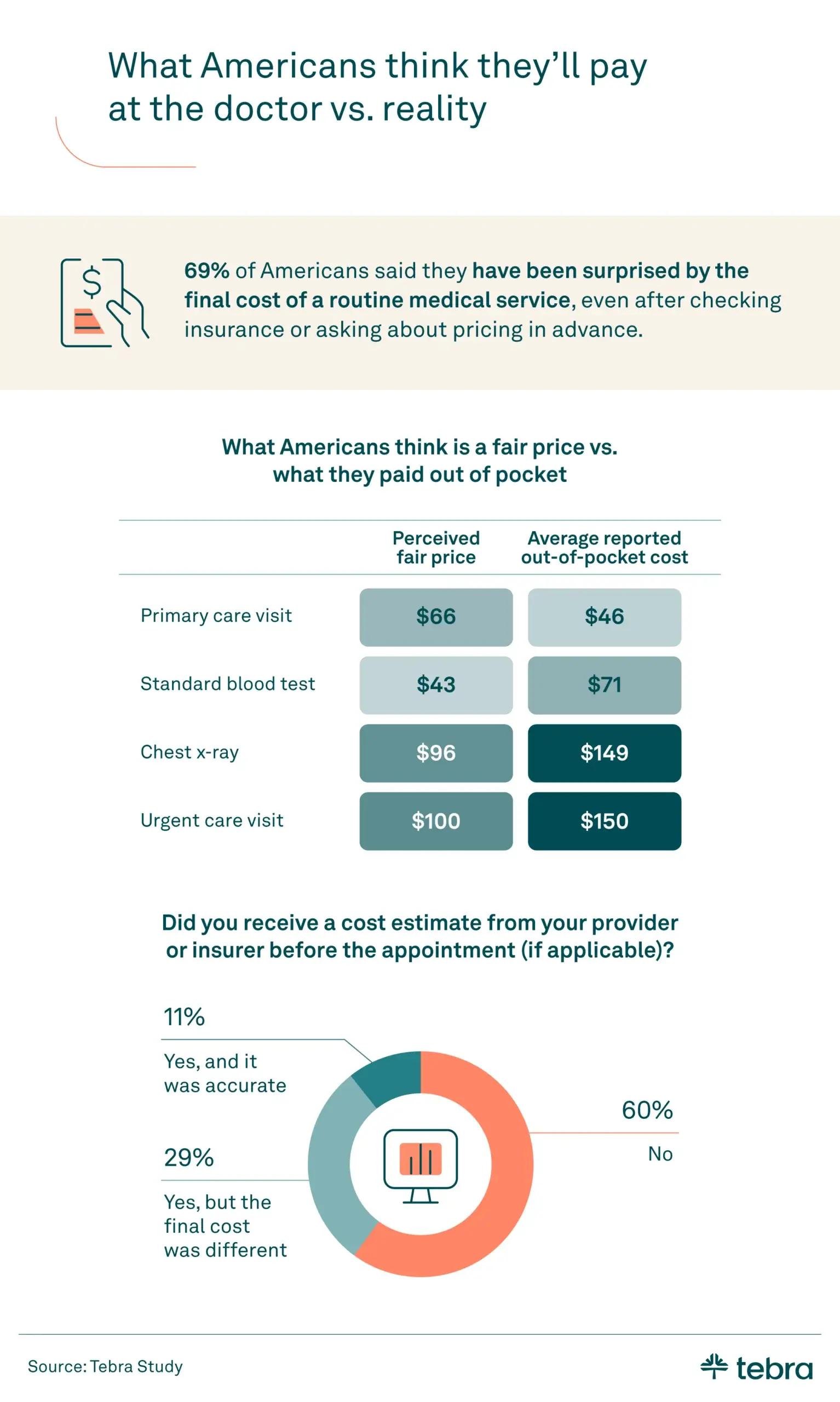
Nearly 7 in 10 Americans (69%) reported being surprised by the cost of a routine medical service, even after checking with their insurance or asking the provider about pricing beforehand. This gap between expectations and reality is not only frustrating but can also lead to delays in care and growing distrust in the system.
The services that most often led to a surprise final cost for patients were:
- Blood work or lab testing: 14%
- Urgent care visits: 12%
- Dental care: 12%
On average, Americans underestimated the cost of routine care by $39. Blood work, in particular, stood out for its price disparity, with out-of-pocket costs averaging 65% more than what patients considered fair.
Medical bills aren't easy to decode
Unexpected costs are only one part of the problem; many patients struggle to navigate complex language and eligibility verification issues that leave them guessing.

Nearly 1 in 3 Americans (32%) said they weren't confident in understanding the charges on their last medical bill. Younger patients, especially Gen Z and Millennials (both at 37%), were more likely to feel confused compared to Gen X (23%) and Baby Boomers (18%). Gen Z (15%) was the most likely to turn to technology, using AI tools or apps to break down the charges.
When patients challenged billing issues, insured Americans (43%) were more likely than uninsured Americans (30%) to dispute charges. Older generations were also more likely to have questioned medical bill costs:
- Baby Boomers: 52%
- Gen X: 51%
- Millennials: 41%
- Gen Z: 23%
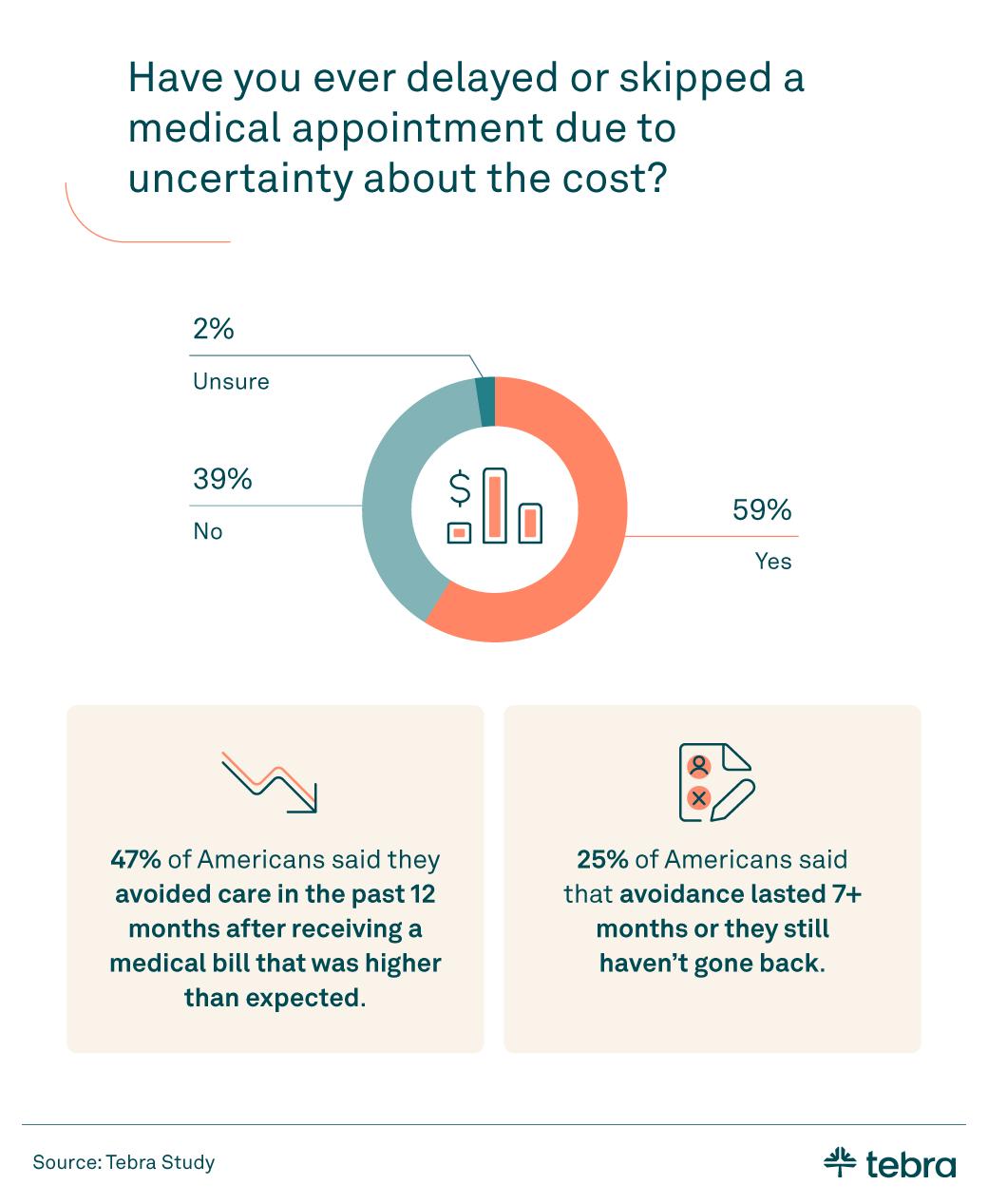
Almost half of Americans (47%) said they avoided care in the past year after receiving a bill that was higher than expected. Among the uninsured, 81% delayed or skipped care due to uncertainty about the cost, compared with 57% of insured individuals.
The care Americans expect to postpone
Widespread cost concerns are leading many people to plan on delaying care in the year ahead.

In 2026, 60% of Americans said they would delay or skip at least one type of medical care due to cost. Among the uninsured, that number jumped to 87%, while 57% of insured individuals expected to do the same.
Here's how this breaks down by generation:
- Baby Boomers
- Dental care (36%)
- Specialist visits (28%)
- Preventive check-ups (21%)
- Gen X
- Dental care (34%)
- Specialist visits (32%)
- Emergency care (18%)
- Millennials
- Specialist visits (37%) (highest of any generation)
- Dental care (34%)
- Mental healthcare (24%)
- Gen Z
- Dental care (34%)
- Specialist visits (34%)
- Mental healthcare (25%) (highest of any generation)
Two-thirds of lower-income Americans earning under $50,000 (66%) expected to delay or skip care in 2026, compared to 59% of middle-income and 49% of upper-income earners.
A lack of understanding about how insurance works may contribute to these decisions. Only 23% of Americans correctly recognized that they would owe the full $1,000 cost of a medical test if they hadn't met their deductible, even if their insurance "covers 80%." This confusion leads many to assume they'll be protected from high costs when they're not.
Rebuilding clarity and confidence in healthcare
Cost confusion can become a barrier to care, trust, and better health. Patients are trying to make informed decisions, but unexpected charges and unclear bills often leave them feeling defeated.
Private practices can lead the way in reducing this confusion by having transparent pricing discussions, providing simple explanations of insurance benefits, and proactively communicating cost expectations. Leveraging digital tools, like patient portals or AI-powered billing breakdowns, may also help bridge the gap between perception and reality.
By making costs clearer and care more predictable, providers can rebuild trust and help more patients get the care they need without hesitation.
Methodology
Tebra surveyed 1,005 Americans to explore what they believe healthcare should cost, what they actually pay, and how surprise bills are affecting their choices. Among them, 91% were insured, and 9% were uninsured. Income groups were defined using the US Census Bureau median household income benchmarks and the Pew Research Center's methodology for identifying lower-, middle-, and upper-income tiers. The generational breakdown is as follows: Gen Z (18%), Millennials (47%), Gen X (25%), and Baby Boomers (10%). Data was collected in January 2026.
About Tebra
Tebra, headquartered in Southern California, empowers independent healthcare practices with cutting-edge AI and automation to drive growth, streamline care, and boost efficiency. Our all-in-one EHR and billing platform delivers everything you need to attract and engage your patients, including online scheduling, reputation management, and digital communications.
Inspired by "vertebrae," our name embodies our mission to be the backbone of healthcare success. With over 165,000 providers and 190 million patient records, Tebra is redefining healthcare through innovation and a commitment to customer success. We're not just optimizing operations — we're ensuring private practices thrive.
Fair use statement
This information may be shared for noncommercial purposes with proper attribution. Please include a link back to Tebra when referencing or quoting this article.





