
- 54% of healthcare professionals say their organization plans to adopt an AI-driven billing system, and 30% already have, reflecting growing automation in revenue cycle management (RCM).
- 64% report insurance claim denials as a major challenge, while 54% cite delays in claims processing.
- 18% spend more than 20 hours per month resolving billing errors, which strains staff time and RCM performance.
- 34% believe practices will expand outsourcing medical billing in 2025 to control costs and improve accuracy.
Medical billing is becoming increasingly complex, creating challenges for providers and patients. Many organizations are adopting AI-driven tools and outsourcing select tasks to improve accuracy and reduce administrative load.
Based on a survey of healthcare providers and patients, this report explores the biggest hurdles, how teams are adapting, and where the market is heading. We also address medical billing costs per claim, common pricing structures used by vendors and in-house teams, and patient statement best practices.
As reimbursement affects every medical practice, we connect operational choices in RCM to real impacts on cash flow. Ahead, you’ll find a simple cost breakdown that covers labor, technology, and A/R delay, along with national benchmarks to help you compare your numbers and spot opportunities to improve.

How providers are addressing billing challenges and industry changes
Medical billing costs per claim are the end-to-end expenses to submit, adjudicate, and collect a claim. They include labor, technology/clearinghouse tools, and A/R delay costs driven by denials and resubmission work.
Some healthcare professionals face persistent hurdles in the billing process that affect financial health and daily operations. To understand what’s changing, we surveyed healthcare providers about their biggest obstacles and the tools they use to solve them.
- The top challenges include insurance claim denials at 64% and delays in claims processing at 54%.
- 18% spend more than 20 hours each month fixing billing errors.
- 22% say high medical billing software or outsourced service costs are a concern; many evaluate the costs of medical billing software to budget accurately.
- 54% plan to adopt AI billing systems within 1 to 2 years, and 30% already have teams testing automation to reduce touches and speed reimbursements.
Stronger front-end work helps. Accurate eligibility checks, clean coding, and timely claim submission cut rework and speed payment. For a practical walkthrough of processing claims, see Tebra’s guide on how to process insurance claims for medical practices. Many teams are also weighing AI and automation options to streamline follow-up with patients and reduce denials.
As delays accumulate, accounts receivable days rise. Longer A/R ties up cash and slows RCM performance, which pressures cash flow for everyday needs. Later in the FAQ, we reference national benchmarks to help you compare your workflow and spot improvement opportunities.
Cost breakdown per claim
Labor: Front-end insurance verification and eligibility, medical coding, clean claim submission, payer follow-up, and denial management and audits. Each touch adds time and expense from the initial patient encounter through final payment. Electronic status checks can save minutes per transaction and reduce phone time.
A/R delay: The cost of capital while medical claims age in receivables, plus extra staff time for resubmission and appeals. Rising denial trends can lengthen cycles and reduce total collections.
Pricing snapshot: Outsourced medical billing services commonly use a percentage of collections or a per-claim rate model. Typical ranges include percentage-based fees of 4–10% and per-claim pricing around $3–$10, with variation by specialty, claim volume, and payer mix. Hourly projects appear for specialized work.
What practitioners expect next
Respondents anticipate 5 trends shaping healthcare billing in 2025:
- More AI and automation
- New compliance requirements
- Faster claims processing
- Better coding accuracy
- Expanded outsourcing for practice management support
Private practices can ease billing challenges by using comprehensive EHR and billing software, along with AI and automation. These tools help reduce errors, cut administrative work, and improve accuracy, allowing providers to focus more on patient care.
Weighing the costs and benefits of outsourced billing
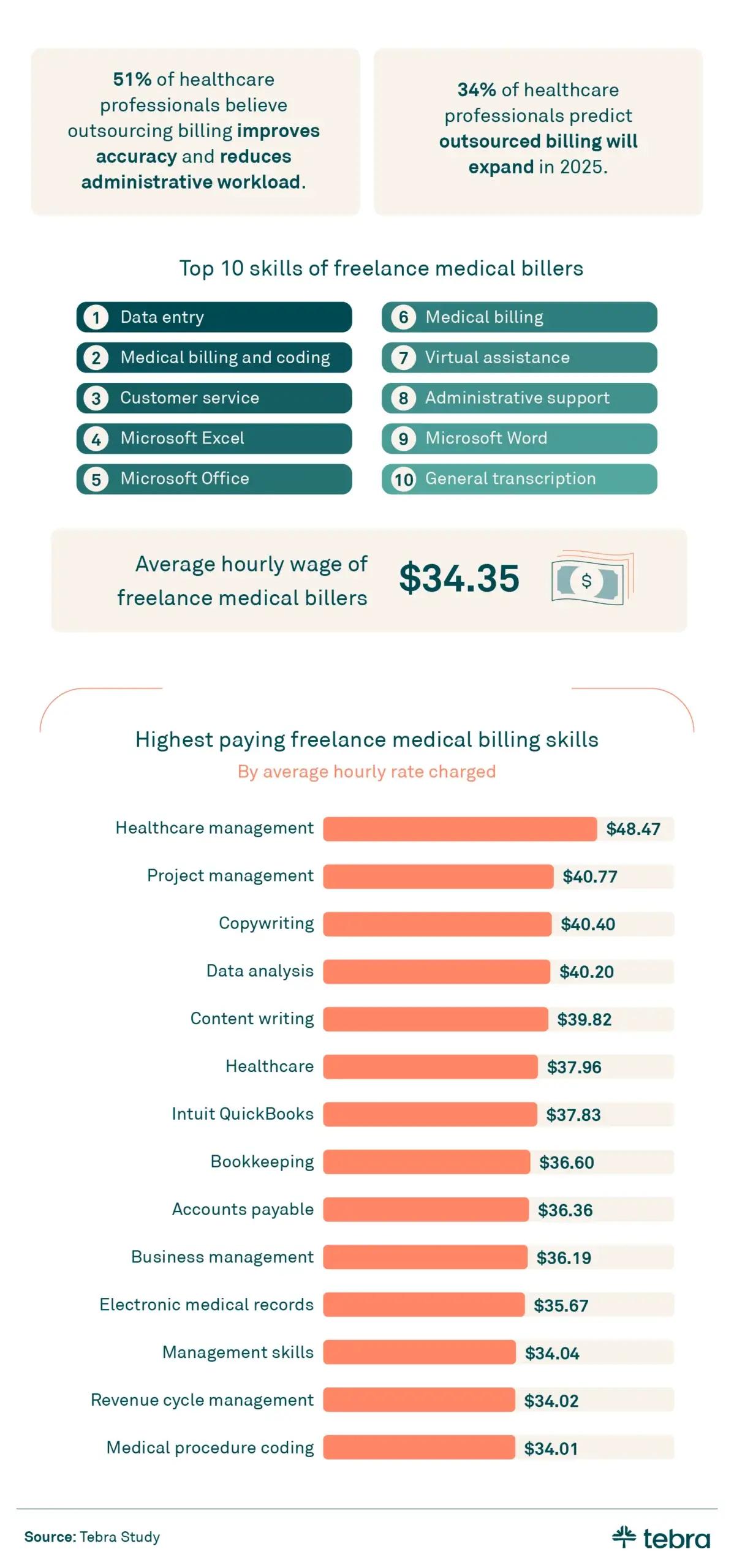
Many medical practices weigh medical billing outsourcing to reduce administrative work and improve accuracy. Understanding freelance rates and how teams view outsourcing helps decide what to keep in-house and what to send to a billing service provider.
- 51% of respondents say outsourcing improves accuracy and reduces workload.
- Freelance billers average $34.35 per hour, with $48.47 per hour for healthcare management tasks.
- 34% believe practices will expand outsourcing medical billing in 2025.
Pricing models at a glance
Vendors use several billing models. Common approaches include percentage-based fees, per-claim fees, and hourly or flat rate options. Ranges vary by specialty, claim volume, and payer mix.
- Percentage of collections: Many medical billing companies price on a share of monthly collections, typically 4–10%.
- Per-claim rate: Low-volume groups may prefer per-claim fees in the $3–$10 range per claim.
- Flat fee or monthly fee: Some opt for a flat fee with monthly minimums. Specialized projects such as credentialing may use an hourly rate. Contracts should clarify any setup fees or hidden fees.
In-house vs outsourced
Use this quick check to compare in-house billing with outsourcing medical billing on control, ongoing costs, and tools, payer follow-up in the billing process, and RCM support from a billing service provider:
- In-house billing: Closer control and visibility; ongoing operational costs for staffing, training, medical billing software, and clearinghouse services. Teams must manage denials, resubmission, and payer follow-up. Integration with EHR software is essential for a clean billing process and steady reimbursements.
- Third-party medical billing: A full-service billing partner can streamline revenue cycle management (RCM), apply benchmarks, and scale capacity for small practices and larger practices. Pricing depends on practice size, geographic location, and service scope. Consider how the vendor supports customer support and reporting.
When evaluating vendors, confirm integration with your EHR software for clean data flow and fewer touches. Make sure the contract spells out the pricing model, any service fee or administrative fees, and how denial management and payer follow-up are handled.
The provider's role in reducing billing confusion
Billing confusion increases admin work for practices and creates stress for patients. Clear patient statements, accurate coding, and timely follow-up improve transparency and reduce disputes. Simple design choices matter. Use plain language, readable line items, and high-quality communications that explain coverage, adjustments, and balances.
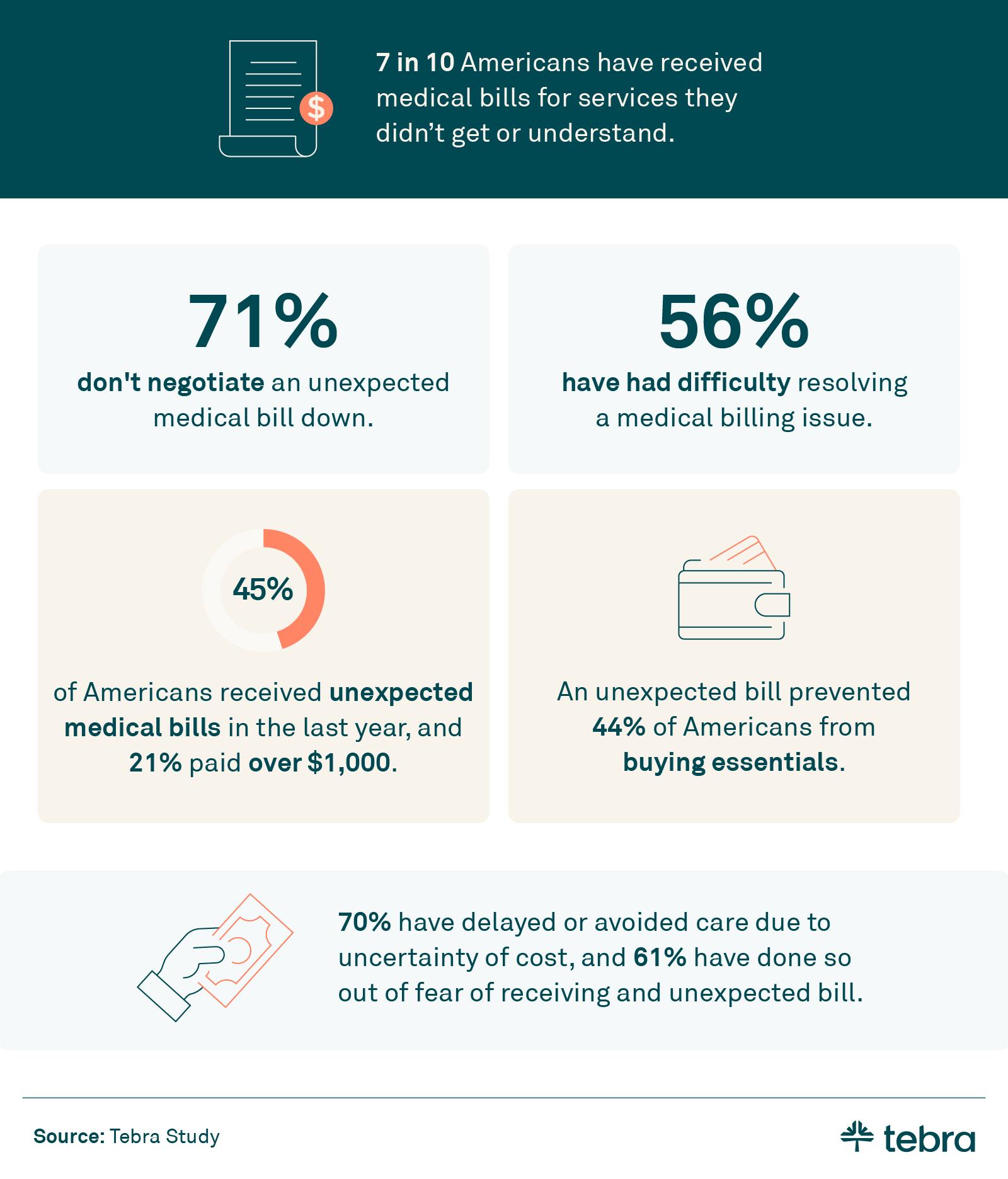
- 45% of patients were surprised by unexpected fees in their medical bills last year.
- In the last year, 21% of patients paid over $1,000 in unexpected medical fees, and more than 1 in 10 (14%) paid over $2,000.
- 44% of patients said a surprise medical bill had prevented them from buying essentials.
- 70% of patients have delayed care due to cost uncertainty, and 61% have done so out of fear of receiving an unexpected bill.
Modern tools help. Real-time eligibility checks and electronic ERAs support cleaner posting and fewer reworks. Itemized patient statements paired with insurance verification at check-in reduce avoidable denials and speed up payment time. Automated reminders and two-way messaging improve patient experience when questions arise.
Teams should align denial management workflows with front-desk tasks, ePrescribing/eRx protocols, and charge capture to prevent mismatch errors. They should also use HIPAA-compliant tools for payment links, estimates, and balances.
Make it easy for patients to ask questions through customer support channels and document resolutions inside the billing process. When these steps are in place, practices spend less time correcting bills and more time on care.
How private practices can stay ahead with efficiency and automation
As medical billing grows more complex, healthcare professionals face challenges like claim denials and processing delays that strain finances and staff time. To adapt, many teams are implementing automation and exploring outsourcing, with more than half planning to add AI tools and over a third expecting to expand external support. These choices reduce manual rework and improve accuracy so staff can focus on patient care.
Tighter integration between EHR systems and practice management tools matters. When schedules, charges, and clinical notes flow cleanly into claims, there are fewer manual touches and fewer handoffs in the workflow. That consistency supports faster payment posting and steadier cash flow.
Private practices that standardize eligibility checks, charge capture, and claim edits see fewer avoidable errors. Centralized work queues, electronic status checks, and automated reminders keep revenue cycle management moving. The result is more predictable operations that are cost-effective without sacrificing service quality.
Methodology
To understand current billing realities, Tebra surveyed 800 Americans and 200 healthcare professionals about experiences, challenges, and tools used in medical billing. The study compares patient views with provider perspectives to surface areas of alignment and friction. Tebra also analyzed more than 1,900 freelance medical biller profiles on Upwork to evaluate skills and the average hourly rate within the healthcare industry.
Freelancer pricing figures reflect median and mean values calculated from that sample, and they apply to both medical practices and broader provider settings. Where relevant, we reference directional benchmarks to contextualize medical billing service rates and related trends. All analyses were reviewed for consistency and clarity before inclusion in this report.
About Tebra
Tebra, headquartered in Southern California, empowers independent healthcare practices with cutting-edge AI and automation to drive growth, streamline care, and boost efficiency. Our all-in-one EHR and billing platform delivers everything you need to attract and engage your patients, including online scheduling, reputation management, and digital communications.
Inspired by "vertebrae," our name embodies our mission to be the backbone of healthcare success. With over 165,000 providers and 190 million patient records, Tebra is redefining healthcare through innovation and a commitment to customer success. We're not just optimizing operations — we're ensuring private practices thrive.
FAQs
Common questions about medical billing costs
- Current Version – Nov 17, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.





