- Delayed care: Over 1 in 3 people have avoided or delayed medical treatment this year due to cost.
- Emergency readiness: Nearly 1 in 3 feel completely unprepared for unexpected medical expenses.
- Clinician concern: 1 in 4 healthcare professionals report significantly increased concern about healthcare costs due to the state of the economy.
- Rising patient burden: The majority of healthcare professionals (77%) foresee increasing financial burdens on patients due to economic conditions.
- Treatment deferral: 63% of healthcare professionals have noticed more patients skipping or delaying treatments because of costs.
In a new year of economic flux, a persistent question returns: How do financial ups and downs affect healthcare affordability and access? Tebra surveyed 800 Americans and 200 healthcare professionals across the United States to understand the real-world impact.
Within the healthcare system, rising healthcare spending and everyday price pressure shape choices for patients, providers, payers, and health plans. People feel the weight of healthcare costs, healthcare expenses, and broader expenditures as they decide when and where to seek care.
Beyond the stress, we look at how people adapt and what could make care more affordable. We explore the cost of healthcare across the US healthcare system, including healthcare expenditures in 2024 and how trends tied to gross domestic product may affect access for patients and clinicians.
What is healthcare cost reduction?
Healthcare cost reduction means redesigning care delivery to achieve high-quality, high-value outcomes at lower costs. Many programs use value-based models, telehealth, and predictive analytics with health information technology (HIT) to streamline workflows and expand preventive care.
Teams also strengthen collaboration, address social determinants of health, and optimize resources to deliver durable cost savings without compromising patient safety.
2024 healthcare perspectives: Navigating costs amid economic changes
Rising costs and clinician shortages point to a worsening US healthcare crisis. Households face higher premiums, growing out-of-pocket costs, tougher deductible burdens, and confusing health insurance choices.
Patients' perspectives on healthcare cost challenges
Affording healthcare in the United States can be challenging during economic uncertainty. Budgets stretch to cover premiums, deductible obligations, and out-of-pocket costs under different health insurance plans. These pressures shape choices and overall affordability for many families.
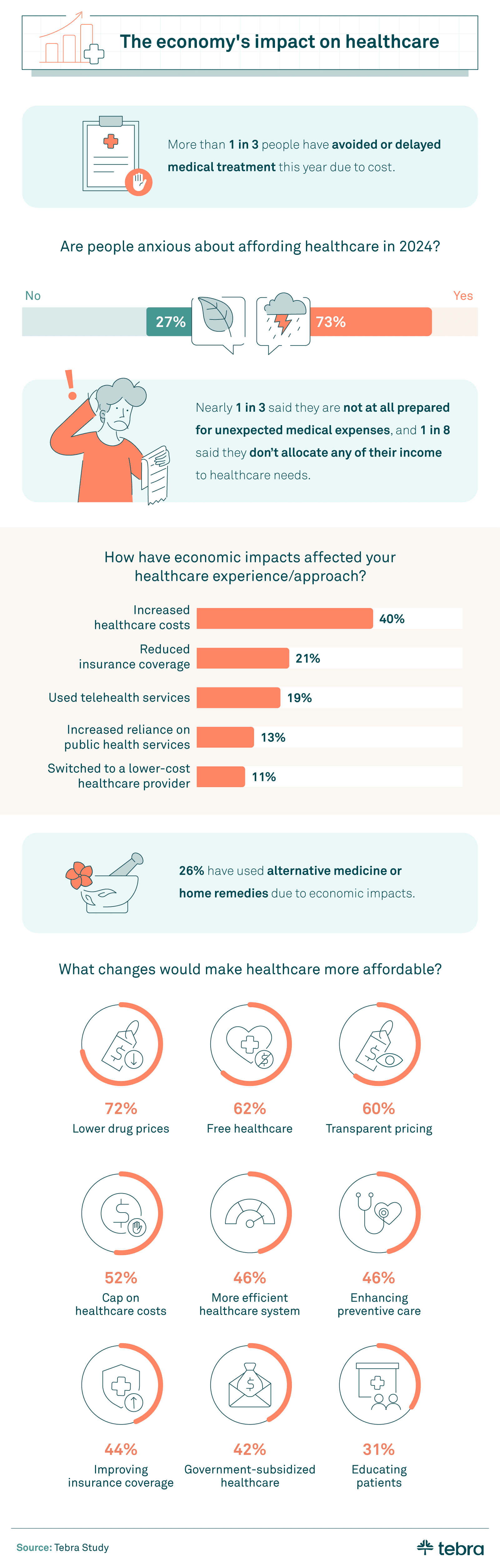
More than a third (36%) of individuals this year delayed or skipped treatment due to cost concerns. For people managing chronic conditions, delayed visits may increase the likelihood of hospitalizations or readmissions, especially when monitoring or medication adjustments are needed.
Anxiety over costs in 2024 is high. Nearly three-quarters (73%) worry about paying for care, and over a quarter (27%) report extreme anxiety. Many also report higher costs across the cost of care, including visits, tests, and prescription drug costs. Nearly 1 in 3 feel unprepared for an unexpected medical bill.
Due to the economy, over a quarter of people (26%) tried home remedies or alternative care instead of traditional visits. About 1 in 5 reduced coverage or chose telehealth appointments, while over 1 in 10 selected a lower-cost provider. Shifts to telehealth, outpatient settings, or lower-priced medical services can offer short-term cost savings.
They may also affect patient outcomes if follow-up or diagnostics are delayed. Patients often discuss trade-offs with clinicians to balance near-term expenses and long-term health.
The top five changes patients believe would make healthcare more affordable are:
- Lower drug prices
- Free healthcare
- Transparent pricing
- Cap on healthcare costs
- More efficient healthcare system
Healthcare professionals' perspectives on rising costs
Patients aren't the only ones concerned about rising healthcare costs. Healthcare professionals also weighed in on how they are adapting to economic pressures. Across healthcare organizations, payers, and health plans, leaders report strain on care delivery and quality of care.
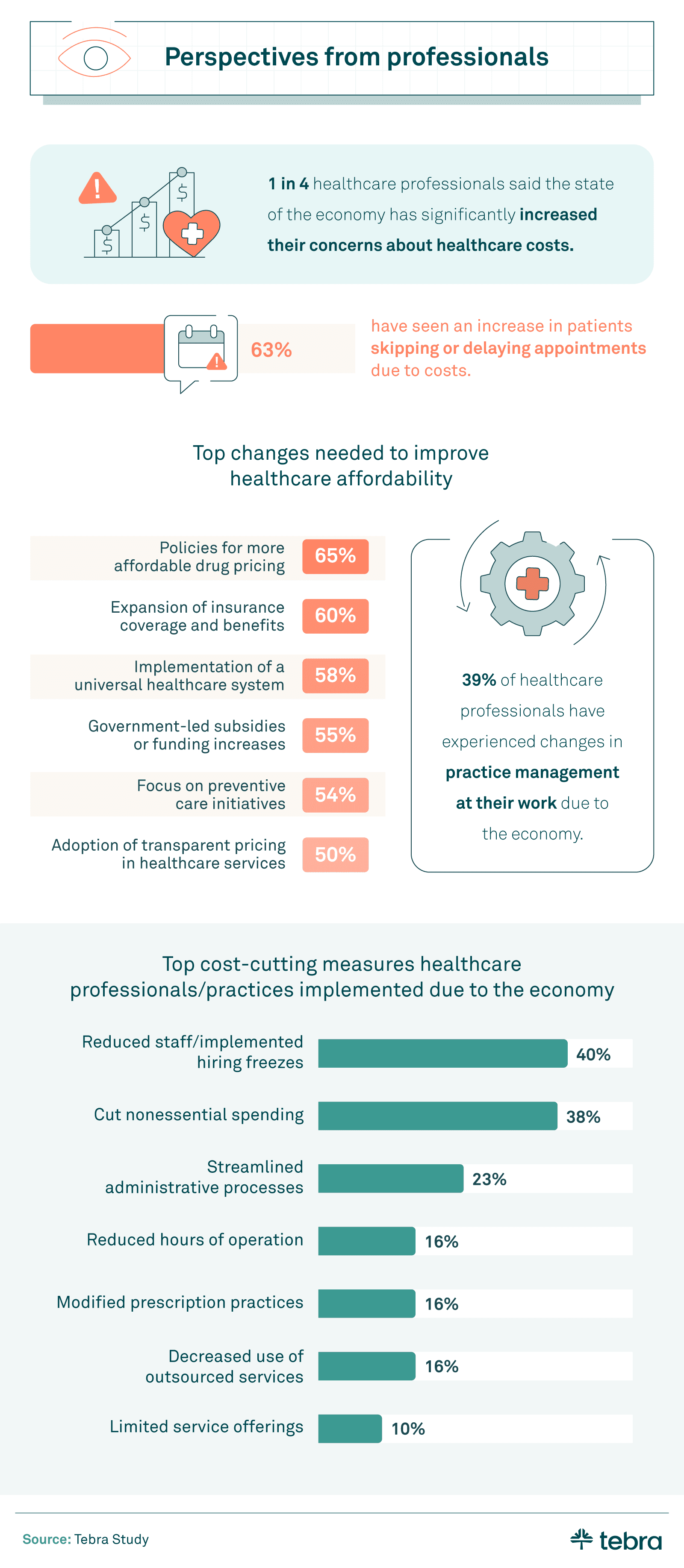
Within the healthcare community, 1 in 4 professionals report increased concern about costs. Well over half (63%) have observed more patients bypassing or postponing treatments due to financial hurdles. Delayed care can raise the likelihood of hospitalizations and readmissions, which may affect patient outcomes and overall health outcomes.
Operational planning has also become harder as Medicare and Medicaid policies evolve within broader health policy changes. Reimbursement pressure and documentation requirements add administrative load for clinicians and can reduce time for direct care.
Teams are testing value-based initiatives and evidence-based interventions to maintain high-value, high-quality care while controlling expenses.
Professionals say the following changes could improve affordability in the United States:
- Drug pricing policies
- Expanded insurance/benefits coverage
- A universal healthcare system
- Government funding
- A focus on preventive care
Top challenges healthcare professionals anticipate due to economic conditions
Healthcare professionals flagged key pressure points as affordability and operational pressures.
- Increasing financial burdens on patients (77%), including higher costs for medical services.
- Navigating insurance and coverage complexities (65%), including cost-sharing rules.
- Escalating costs of running a healthcare practice (55%).
- Upholding high-quality care with limited resources (52%).
- Adapting to technological advancements and limitations (19%).
Healthcare costs' future effect on patient outcomes
The economic currents of 2024 touched every part of care. Patients have delayed visits as affordability worries grew and the cost of care climbed. These choices can influence patient outcomes and broader health outcomes, especially for those with chronic conditions who miss monitoring or medication checks.
Skipped appointments may lead to preventable hospitalizations or readmissions. Practices are responding with targeted intervention and evidence-based changes in care delivery to keep people on track, including support for beneficiaries in Medicare and Medicaid.
However, the results are still sobering: Financial constraints impede the health of both patients and practitioners.
Methodology
Tebra surveyed 800 Americans and 200 healthcare professionals on January 24, 2024. Findings reflect respondents' views at that time and may inform health policy discussions about affordability, access, and spending.
About Tebra
Tebra was formed in 2021 when Kareo and PatientPop joined forces. It provides an all-in-one EHR, billing, and patient engagement platform for private practices. The platform supports online scheduling, ePrescribing, documentation, claims, patient payments, reputation management, and digital communications in one system. Tebra helps practices deliver modern care and operate efficiently from intake to follow-up.
Fair use statement
Feel free to share these findings for noncommercial use, but please remember to attribute the source by linking back to this page to uphold the integrity of the information.
Common questions about healthcare costs
- Current Version – Oct 28, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.