The complete guide to patient engagement for independent practices
Why is patient engagement important, and how can independent practices improve it? Discover essential patient engagement strategies and resources here.
Overview
- Patient engagement, defined as patients feeling involved in, responsible for, and empowered in their healthcare journey, leads to better health outcomes, cost savings, and higher patient satisfaction.
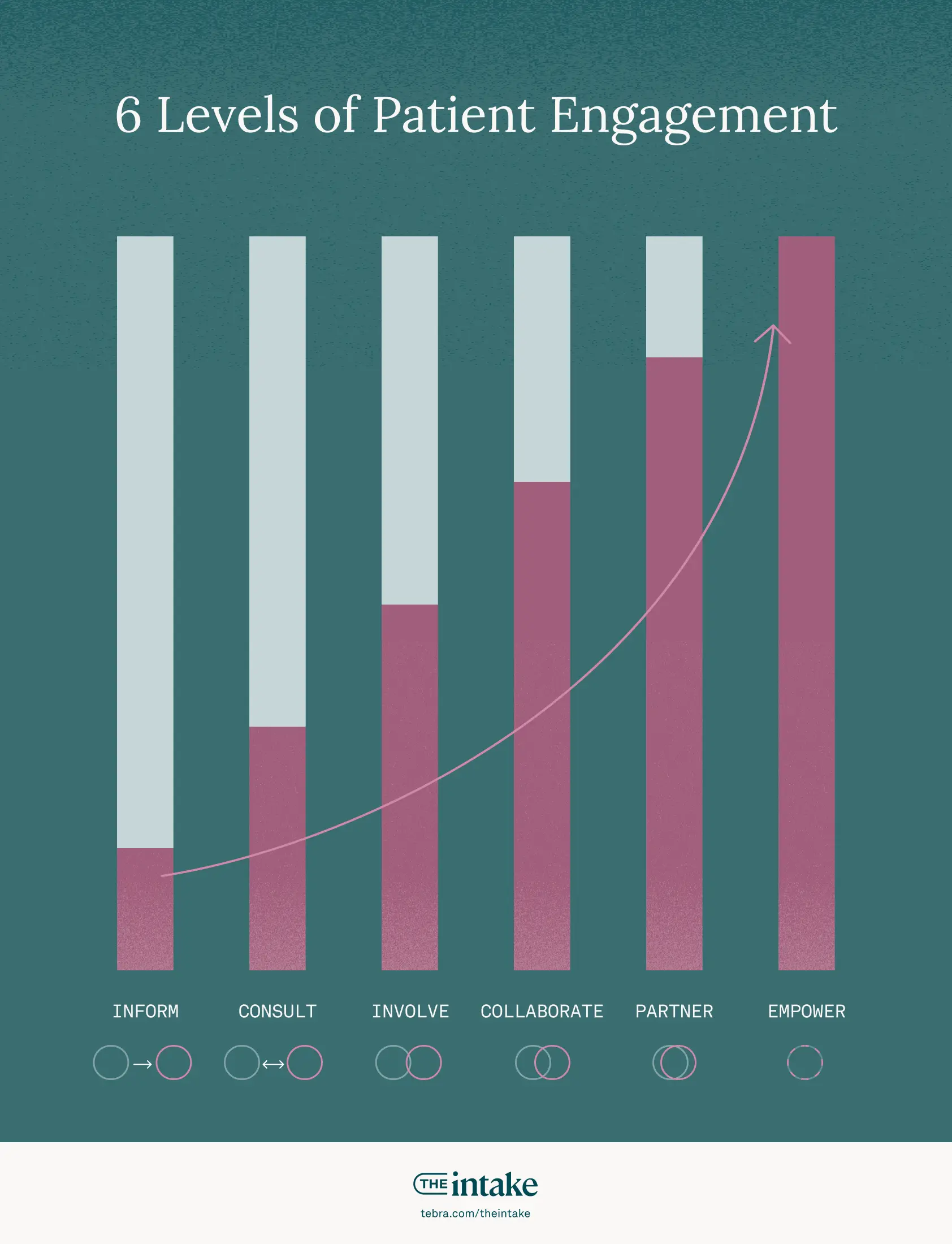
- There are 6 levels of patient engagement, ranging from informing patients to fully empowering them, and practices can implement strategies like clear communication, shared decision-making, and leveraging digital tools to improve engagement.
- Measuring patient engagement through tools like the Patient Activation Measure (PAM®) and practice metrics is crucial, and patient engagement software can help independent practices meet patients’ expectations for a modern healthcare experience.
The most successful practices have patients who are active partners in their own care. This is the essence of patient engagement — a strategy that leads to better health outcomes, higher satisfactiodin, and a more efficient practice.
The concept is not longer limited to the relationship between a provider and a patient. True patient engagement means a person is proactively involved and empowered throughout their entire healthcare journey, from appointment booking to following care plans.
This shift means that engagement is influenced by every interaction a patient has with your practice, including every team member and every digital tool you provide. Below, we offer a comprehensive guide to foster this partnership and build a more successful practice.
| Patient engagement is when patients feel involved, responsible, and empowered in their care across every touchpoint. Independent practices can raise engagement by communicating clearly, using shared decision-making, offering digital access (online scheduling, portals, texting), sending timely follow-ups, and removing friction so patients can act confidently between visits. |
Why is patient engagement important?
Many patients today feel they are not meaningfully involved in their treatment plans or condition management. Some do not fully comprehend their diagnosis or treatment options, while others lack the necessary tools, resources, or knowledge to effectively self-manage their care between visits. A 2021 peer-reviewed article named "personal" factors — including a lack of self-care knowledge and the difficulty of changing habits — as a top barrier among patients with heart failure.


"Patient engagement has been found to have many benefits for the patients themselves, as well as for the organizations that support and facilitate it"
“Patient engagement has been found to have many benefits for the patients themselves, as well as for the organizations that support and facilitate it,” says Jan Oldenburg, consumer health information strategy and personal health engagement expert, author of several books, and founder of Participatory Health Consulting.
Engaged patients have higher quality care and cost less because they have the motivation, comprehension, and skills to adhere to their care plans. This engagement encourages proactive behavior in seeking appropriate follow-up care and maintaining a healthy lifestyle.
Patient engagement is closely tied to patient activation, which Judith Hibbard, founder of the patient activation measure (PAM) — one of the most commonly used methodologies used to assess patient engagement — described as “understanding one’s own role in the care process and having the knowledge, skills, and confidence to take on that role.”
Engaged patients:
- Understand their risk factors and conditions
- Know how to access their medical records
- Are comfortable asking questions
- Are confident making care decisions alongside providers
- Proactively seek support and treatment
3 ways engaged patients fare better
When patients transition from passive recipients to active partners in their care, the results are clear for their health and your practice's performance:
- Better treatment adherence. Engaged patients are more likely to follow treatment plans, take medications as prescribed, and participate in preventative care. This active involvement directly leads to better clinical outcomes and a lower risk of complications.
- Better long-term health outcomes. Engaged patients who practice effective self-management and preventative care experience fewer acute health events. This not only improves their quality of life but also solidifies your practice's reputation for delivering high-quality, effective care that keeps patients healthier.
- Increased operational efficiency. Patients who actively use digital patient engagement tools, such as online scheduling platforms and secure messaging systems, demonstrate higher appointment adherence and more proactive communication with their healthcare providers. This reduces costly no-shows, decreases the administrative burden on your staff, and protects practice revenue.

What are the 6 levels of patient engagement?
Patient engagement is not a static measurement or a box to tick yes or no. Rather, there are various levels at which providers can work to engage patients in their own healthcare journeys.
Based on the 6 stages of stakeholder involvement, which is often used in community advocacy and also the business and finance industries, the 6 stages of patient engagement are similarly a spectrum. Each step denotes greater patient involvement in their own health.
- Inform. Providers share details by telling or informing patients about their health status, treatment options, and care plans.
- Consult. Providers share information and solicit patient opinions, input, and preferences, but providers remain the primary decision-makers.
- Involve. Providers more actively involve patients in a shared decision-making process.
- Collaborate. Providers work alongside patients to collaboratively design treatment plans. Patients’ perspectives and preferences are fully integrated into treatment planning.
- Partner. Providers and patients collaborate as partners to manage conditions and develop treatment plans. Patients share decision-making alongside physicians and other members of their care teams.
- Empower. Patients are fully activated and engaged in their healthcare. They proactively lead their healthcare journey and have the knowledge, confidence, and skills to self-manage their conditions and health.
What are the ways patient engagement motivates patients?
The more engaged patients are, the more likely they are to be self-motivated in their healthcare. A 2020 peer-reviewed study noted that the “engaged patient has a strong motivation to become more knowledgeable and more powerful.”
This could be because the same techniques that help support patient engagement — active listening, open-ended questions, affirming a patient’s perspective — help emphasize their intrinsic motivations in care conversations. Once a clinician has identified what those motivations are, they are better able to work alongside patients to co-create care plans and make decisions, which can help promote shared decision-making.
The process of advancing through the 6 steps of patient engagement can serve to motivate patients, too — as they acquire more knowledge, skills, and confidence.
7 patient engagement strategies private practices can implement
Here are 7 actionable strategies you can implement to build a more engaged patient population and a more successful private practice.
1. Prioritize clear and empathic communication
Effective engagement begins with exceptional communication. This means practicing active listening to ensure patients feel heard, and ditching medical jargon in favor of clear, simple explanations. Always provide written instructions — in a patient's preferred language when possible — to improve understanding and adherence after the visit.
2. Engage patients in shared decision-making
Move from instructing patients to collaborating with them through shared decision-making. This involves working together to create personalized treatment plans that reflect a patient’s unique goals, values, and lifestyle. When patients help build the plan, they are far more invested in the outcome.
3. Streamline the patient experience with digital tools
Patients expect the same digital convenience from their healthcare provider that they get in their day-to-day lives. Tebra's 6th annual Patient Perspectives survey confirms that certain tools significantly improve their experience. Nearly half of all patients value online access to lab reports (48%) and automated appointment reminders (47%), while many also prioritize the ability to book (43%) and reschedule (40%) appointments online and communicate through secure messaging (39%). Implementing these tools automates the patient journey and meets modern expectations.
4. Offer telehealth for convenience and access
Part of engaging patients means meeting them where they are. For many, telehealth is a more convenient and accessible option for routine follow-ups, medication checks, and consultations. Tebra’s data shows that a growing number of patients — 18% in 2025, compared to 9% in 2024 — will leave a healthcare provider over lack of telehealth options, making it a critical tool for a modern, patient-centric practice.
5. Support patients between visits
Engagement shouldn't end when a patient leaves your office. Use your patient portal or secure text messaging to maintain an open line of communication. Proactively check in, answer questions, and provide encouragement to help patients adhere to care plans. A 2022 JAMA study found that simple text message outreach reduced a patient's risk of hospital readmission within the next 30 days by 41%.
6. Measure engagement to personalize care
Go beyond one-size-fits-all care by using formal assessments to understand patient activation. A tool like the PAM provides a baseline of a patient’s confidence in managing their health, allowing you to tailor your approach for maximum impact.

7. Request patient feedback actively
Regularly ask patients for feedback about their experience. This has a powerful dual benefit: it provides your practice with testimonials for social proof and also gives you invaluable, actionable insights to improve your operations. More importantly, it shows patients you value their voice.

How do private practices know if their patient engagement strategies are successful?
Understanding whether your patient engagement strategies are working requires a clear way to measure their impact. The most effective approach combines a formal, clinical standard with real-time data from your practice operations.
The validated standard: The patient activation measure
For a more formal assessment, the patient activation measure (PAM) is a widely validated tool to assess a patient's knowledge, skills, and confidence in managing their own health. Developed by Judith Hibbard, it assigns a score that helps you understand where a patient is on their journey, from "disengaged and overwhelmed" to "active self-manager." Higher PAM scores are directly correlated with better health outcomes and lower costs, making it the foundational metric for measuring true patient activation.
A framework to measure your practice's patient engagement
While PAM provides the clinical benchmark, your daily operational data offers a real-time pulse on engagement. Use the framework below to track these key indicators, understand why they matter, and set targets for improvement.
| Measure | Why it matters | Example target* |
| Portal adoption and use | Provides a direct line for communication and patient self-service. | >70% patient enrollment; increasing monthly logins |
| No-show and cancellation rate | Acts as a key proxy for pre-appointment engagement and practice efficiency. | Decrease rate by 20% vs. your baseline |
| Message response time | Builds trust and shows patients you are accessible and responsive to their needs. | <1 business day |
| Medication adherence | Directly tied to better health outcomes and helps reduce costly readmissions. | Increase in pharmacy sync or refill rates |
| Billing completion | Indicates a positive and frictionless post-care financial experience for patients. | Increase in the share of payments made online |
- Portal adoption and use: Are patients actively using your portal for scheduling, messaging, or accessing health information? High enrollment and consistent use indicate strong digital engagement.
- Website traffic: Traffic to your practice’s website is another way to measure engagement. Look at metrics such as: How many people visit your website monthly? How long do they stay? What information are they looking at or searching for? Are your numbers going up or down?
- Unpaid balances: Engagement extends to financial interactions. Fewer unpaid balances often correlate with patients who feel supported by a streamlined billing process with price transparency and easy online payment options.
- Patient cancellation rates: Engaged patients are more likely to attend their appointments. High no-show rates can signal disengagement and may point to issues with wait times or inconvenient rescheduling options. Tebra's free guide to addressing no-shows and cancellations can help you identify and tackle issues.
Don't forget qualitative feedback
Beyond these metrics, your patient feedback and online reviews are a direct qualitative line to the patient experience and can help you pinpoint successes and concerns. Tools like Tebra’s AI Review Replies can help you respond to new reviews, good or bad, within seconds. AI Review Insights gives you the full story behind the feedback to catch issues early and improve patient satisfaction. Learn more in the video below.
What resources can private practices use to improve patient engagement?
Building a more engaged patient population is one of the most effective ways to create a thriving, resilient practice. It’s a continuous process of improving communication, leveraging technology, and empowering patients to become active partners in their own care.
As you implement these strategies, the following resources can provide deeper insights and support:
- The ONC Patient Engagement Playbook provides comprehensive information on using technology, especially patient portals, to support your patient engagement efforts.
- AHRQ provides free tools and resources for providers, patients, and families. It also offers a helpful PDF aimed at supporting patients and family engagement in hospitals, but many of the tips are applicable to independent practices, too.
- The CDC’s patient engagement page features research-backed information and actionable tips. Its website also makes it easy to access other resources on adjacent topics.
While these resources provide the framework, the right technology brings your strategy to life. Tebra's intuitive, all-in-one platform is designed to streamline tasks, simplify scheduling, and hear directly from your patients. Book a demo today.
FAQs
Frequently asked questions
Engagement is an active partnership between a patient and their provider to improve health outcomes. It expands beyond the office visit to include shared decision-making, consistent communication, and empowering patients to be active in their own care.
You might also be interested in
Learn how to create a seamless patient experience that increases loyalty and reduces churn, while providing personalized care that drives practice growth in Tebra’s free guide to optimizing your practice.
- Current Version – Sep 25, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.
- Sep 23, 2025Written by: Ryan YatesChanges: This article was updated to include the most relevant and up-to-date information available.






