Electronic health records (EHRs) are at the core of healthcare’s digital transformation, replacing traditional paper-based systems with streamlined, data-driven tools. According to HealthIT.gov, over 75% of office-based clinicians and 96% of hospitals in the United States use an EHR system.
EHRs are designed to enhance efficiency, improve patient outcomes, and simplify compliance — yet many providers still struggle with usability and integration challenges. Providers often feel frustrated because their EHRs promised them flexibility and efficiency, but what they've got is rigid and inefficient.
However, when effectively implemented, EHR software can automate key processes, enhance patient engagement, improve health outcomes, and boost operational margins. They let healthcare professionals and care providers focus more on patient care and less on administrative tasks.
Let's learn how to make an informed decision about your practice's EHR.
| Overwhelmed by EHR options? Get expert tips for evaluating systems and making the right decision for your practice. |
What is an EHR?
An electronic health record is a digital system that securely stores and organizes a patient's essential health information, providing a comprehensive view of their overall health.
| An electronic health record is a digital system that securely stores and organizes a patient's essential health information, providing a comprehensive view of their overall health. |
Compared to EMRs (electronic medical records), which focus solely on a patient's medical history, EHRs include a broader scope of information.

What's in an EHR record?
EHR records commonly include:
- Patient contact information: Name, address, date of birth, contact details, insurance information, and emergency contacts.
- Demographics and social determinants of health (SDOH): Age, gender, race, ethnicity, income level, education, employment status, housing stability, and access to transportation to provide a holistic view of potential health risks and to promote targeted interventions.
- Medical history: Past illnesses, surgeries, immunizations, family history, and social habits (e.g., smoking, alcohol use).
- Medications: Current and past prescriptions, dosages, and allergy records.
- Lab results: Blood tests, imaging scans, pathology reports, and specialized tests.
- Vital signs: Blood pressure, heart rate, temperature, respiratory rate, oxygen levels, and height/weight.
- Medical encounters: Progress notes, diagnoses, referrals, and care plans from various providers.
- Orders and prescriptions: Medications, therapy instructions, follow-up care, and emergency guidelines.
- Procedures: Details on surgical or medical procedures and rehabilitation efforts.
- Risk factors: Lifestyle habits, occupational hazards, and environmental exposures.
- Care plans: Chronic disease management, preventive care, and behavioral health strategies.
- Patient-reported outcomes (PROs): Subjective experiences about quality of life and physical functioning, typically captured through surveys or questionnaires, to personalize treatment plans and empower shared decision-making.
- Genomic data: Genetic information to pave the way for personalized medicine. This might include genetic risk assessment and preventive care based on individual predispositions.
EHRs enable authorized healthcare providers to securely access, share, and coordinate patient care. They improve communication, reduce errors, and allow for large-scale data analysis to advance treatments and enhance healthcare delivery.
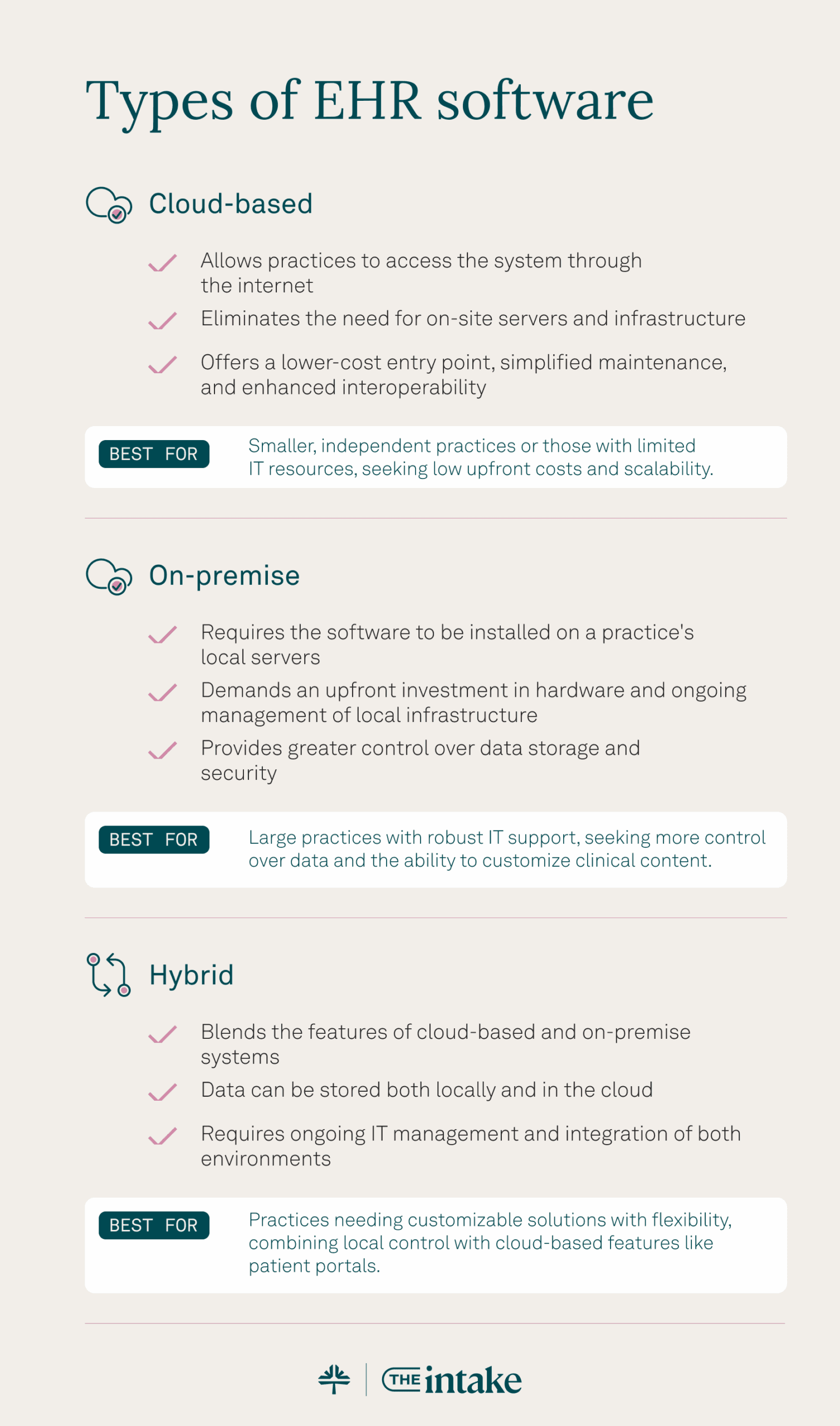
Types of EHR software
EHR software comes in various forms: cloud-based, on-premise, and hybrid. Each cater to different practice needs, budgets, and technical capabilities. Understanding the features and benefits of these 3 primary types can help your practice determine the best option.
Cloud-based EHRs
Cloud-based EHRs, also known as software as a service (SaaS) solutions, allow practices to access the system through the internet. These systems eliminate the need for on-site servers and infrastructure, offering a lower-cost entry point, simplified maintenance, and enhanced interoperability for seamless data sharing across networks.
Best for: Smaller, independent practices or those with limited IT resources, seeking low upfront costs and scalability.
On-premise EHR software
While less common now, on-premise EHRs are still used by some healthcare organizations, particularly larger hospitals or health systems with specific security or customization requirements. However, even traditionally on-premise vendors are increasingly offering cloud options.
On-premise EHRs require the software to be installed on your practice's local servers. This model demands an upfront investment in hardware and ongoing management of local infrastructure but eliminates recurring subscription fees. However, on-premise systems also provide greater control over data storage and security.
Best for: Large practices with robust IT support that want more control over data and the ability to customize clinical content.
Hybrid EHR systems
Hybrid EHRs blend the features of cloud-based and on-premise systems. Data can be stored both locally and in the cloud, offering a balance of flexibility, control, and scalability. While this model supports greater customization, it requires ongoing IT management and integration of both environments.
Best for: Practices needing customizable solutions with flexibility, combining local control with cloud-based features like patient portals.
| Love content like this? Join thousands of independent providers who receive our weekly newsletter with tips on running a more efficient, profitable practice. Sign up for the newsletter. |
EHR features to look for
Choosing the right EHR system is crucial for smooth operations and quality patient care. At Tebra, we know that common pain points in EHRs include excessive clicking, data transfer hassles, and lack of specialty-specific features.
With this in mind, make this checklist your go-to when you're comparing EHR systems:

- User-friendly interface: Features like pre-populated templates, text shortcuts, and drag-and-drop functionality enable faster documentation.
- Seamless patient record management: Integrated demographics, medical history, medications, allergies, immunizations, lab results, imaging reports, and progress notes support efficiency.
- Robust clinical decision support: You'll want evidence-based guidelines, drug interaction alerts, and reminders for preventive care.
- Secure messaging: HIPAA-compliant messaging with patients and other providers is crucial.
- eRx (electronic prescriptions): Send patient prescriptions directly to pharmacies to reduce errors and delays.
- Automated appointment scheduling and reminders: Medical scheduling software and automated appointment reminders benefit both patients and staff.
- Reporting and analytics: Customizable reports support quality improvement, population health management, and financial tracking.
- Interoperability: Easily exchange data with other healthcare systems and laboratories.
- Mobile access: Remote access creates flexibility and responsiveness.
- Scalability: A system should evolve with your practice.
- Training opportunities: Look for a vendor that offers university classes.
- Implementation and support: Consider implementation, ongoing support, and vendor responsiveness to user needs.
- Affordability: Evaluate pricing models, subscription options, and potential hidden costs.
- MACRA/MIPS management: Automated MIPS reporting and tracking systems help you earn the most in positive adjustments.
- PDMP for controlled substance monitoring: Tebra's PDMP enables EPCS-enrolled providers to query their state's PDMP when ePrescribing a controlled substance.
- ONC certification: A cloud-based, ONC-certified EHR supports your entire workflow and simplifies the patient experience.
- Customizable treatment plans: Build-your-own treatment plans can improve practice synchronization, kickstart treatment options, and enable clinical decision-making that guides patients toward their goals.
Tebra's EHR software platform is a modern, certified EHR designed to equip today's provider with clinical tools that support rather than interfere with patient care. This includes all the innovative features your practice needs, from robust clinical charting and streamlined patient documentation to a comprehensive view of the patient and their history, eLabs, telehealth, and more.
Transforming healthcare with Tebra's EHR software
The right EHR system can revolutionize private healthcare practices. From streamlining workflows and enhancing patient engagement to improving care coordination and achieving regulatory compliance, EHRs are invaluable tools for modern healthcare. They empower providers to focus on what matters most — delivering high-quality care to patients.
At Tebra, we understand the unique challenges faced by private healthcare practices. That's why we've built a cloud-based, all-in-one EHR and billing platform that combines cutting-edge AI and automation to drive growth, streamline care, and boost efficiency.
Our solutions, like online scheduling, reputation management, and digital communication tools, help practices thrive in a competitive industry.
Empower your practice with a reliable partner that's redefining healthcare. Visit Tebra.com to learn more and take the next step toward transforming your practice today.
You might also be interested in
- EHR vs. EMR: What’s the Difference? — Understand the key distinctions so you can choose the right system for your practice.
- How EHRs and Healthcare Technology Improve Efficiency — Learn how modern EHR systems streamline workflows, save time, and reduce administrative overhead.
- Want to see an EHR in action? Book a Free Demo and experience how the right system can transform your practice!
- Current Version – Sep 12, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.
- Aug 18, 2025Written by: Jean LeeChanges: This article was updated to include the most relevant and up-to-date information available.
- Feb 21, 2025Written by: Becky WhittakerChanges: This article was updated to include the most relevant and up-to-date information available.






