Overview
- Online appointment booking and automated reminders enhance patient experience and operational efficiency. These tools meet evolving patient expectations for convenience and directly contribute to practice profitability.
- While technology offers significant benefits, maintaining human interaction is key. Thoughtful policies and adaptive communication strategies are necessary to meet patients’ needs without alienating them.
- Effective communication channels and active listening are vital for patient satisfaction and retention. Streamlined administrative tasks and user-friendly EHR systems enable providers to better understand and engage with patients.
For busy medical practices, profit isn’t always about growing your patient base; it’s about optimizing patient scheduling and retention to maximize clinician use.
Retaining patients isn’t just good economics. Stable patient relationships make private practice emotionally rewarding. But the nuances of scheduling — along with managing cancellations and reschedules — can drive a wedge in those relationships.
Patient expectations around scheduling, convenience, and their overall experience are changing quickly. In our recent survey, hundreds of patients shared waiting-room horror stories. Common themes emerged: anxiety about exposure to sick people, especially since the arrival of COVID-19; concerns that the practice did not respect their time; annoyance about no-show fees; and disruptions due to last-minute rescheduling after they’d taken time off work.
In a landscape where patients have rising expectations and more options for meeting healthcare needs, retention is critical for not just patient health but also practice performance.
Technology offers new answers to many of these old problems: self-service scheduling and test reminders reduce no-shows, and telehealth can alleviate some waiting room concerns. Providers can automate patient follow-up communications and provide health results and treatment plans digitally.
In this explainer, you’ll find everything you need to know about:
- Patient scheduling and appointment reminders
- Driving more patient engagement
- Boosting patient satisfaction
- Building effective patient retention programs
How to improve the patient scheduling process
Patient scheduling is a key factor in loyalty — and profits. Being available, communicating well, and convenience rule the way.
Today, there are many ways to improve patient scheduling: understand what patients want, know where they’re flexible and where they aren’t, communicate better, and make the experience more convenient. This article will share new best practices for patient scheduling.
Digitization of patient experience: Bring the patient scheduling process online
Online patient scheduling may be the biggest, easiest upgrade for patients — and your staff.
For medical practices that haven’t invested in online scheduling, these are the key benefits:
- 61% of patients prefer to schedule appointments online, and are frustrated when practices don’t offer it.
- Digital patient scheduling saves hours of staff time each week. Over half of practices spend more than 10 hours a week on scheduling calls (booking appointments and reminders). Some spend more than 30 hours a week.
- Integrating digital patient scheduling with sites like Google and Yelp removes the friction between patients searching for a provider and booking an appointment.
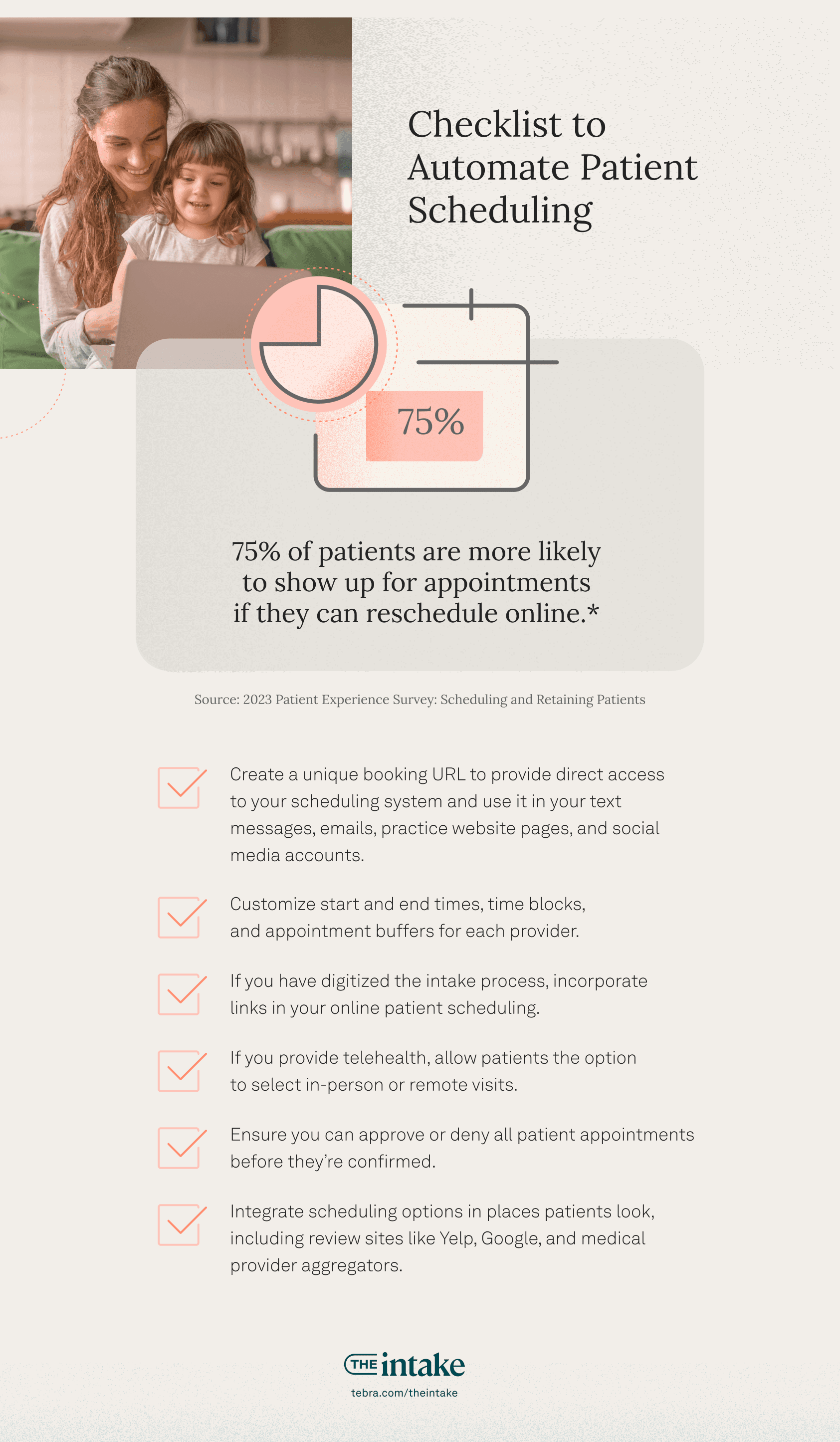
In addition, offering convenient 24/7 rescheduling can prevent no-shows. Our survey shows 75% of patients are more likely to show up for appointments if they can reschedule online.
If you’ve already automated patient scheduling, make sure you’re using it to its full potential:
- Create a unique booking URL to provide direct access to your scheduling system and use it in your text messages and emails. Post a link in your practice website and social media accounts.
- Customize start and end times, time blocks, and appointment buffers for each provider.
- If you have digitized intake, incorporate links in your online patient scheduling. If your clinical and administrative systems are integrated, patient forms can be automatically added to your EHR.
- If you provide telehealth, allow patients the option to select in-person or remote visits.
- Ensure you can approve or deny all patient appointments before they’re confirmed.
- Integrate scheduling options in places patients look, including review sites like Yelp and Facebook, Google, Healthgrades, and medical provider aggregators.
Let patients see other providers if their main one is booked
Patients want to get in for appointments quickly — if they can’t, 50% say they would consider switching doctors. It’s best for you and your patients if they stay with your practice. Your practice already has their medical history, and you’re in a better position to encourage follow-up appointments.
One tip for getting patients in faster is to consider allowing them to see another provider if their normal one isn’t available. 76% of people say they’d be comfortable seeing another provider.
Automate patient appointment reminders
Automated appointment reminders make a significant impact on patient no-show rates: after receiving reminders, patients are more likely to show up for appointments or to reschedule in advance. Patients should routinely receive a reminder a week or so before an appointment scheduled far ahead.
In our recent survey of medical providers, 79% used appointment reminders to reduce no-shows.
Some medical practices remind patients manually by phone, but the pickup rates are low — 67% of people don’t answer unknown phone numbers as a rule — and the process is intensive. Dynamic patient reminders include links to reschedule appointments, making this the easiest and most convenient way for patients to reschedule on their own time.
There are several ways to deliver automated patient reminders: calls, text/SMS, and email. There are pros and cons for each.
Automate patient reminder phone calls
Automated appointment reminder calls are more time- and cost-effective than manual calls — but may still lead to interactions when patients have to cancel or reschedule. Digital communications like email and text can include self-service links.
Younger demographics are less likely to answer phone calls, especially if they don’t know the number, whereas Gartner reports text open rates of 98% — as long as the number you have on file is a mobile. In addition, patients need to opt in to receive text messages, which means you might need to use a combination of call, text, and email to reach patients according to their device types and communication preferences.
Automate patient reminder texts and SMS
Automated text reminders are the gold standard for decreasing patient no-shows. Tebra’s 2023 Patient Perspectives report showed 51% of patients would like a text for an upcoming appointment reminder (vs. 23% by phone). However, legal standards for text messaging permissions (including standard consumer protections and HIPAA rules) means automated SMS reminders have to be managed carefully.
You need consent to send text or SMS reminders — general consent, as for all business-to-consumer activity. And while multiple automated reminder texts can be effective in decreasing no-shows more than a single reminder, you run the risk of annoyed patients revoking consent, forcing you to remind them in other ways.
Patient consent for medical practices must also meet HIPAA standards. Texting PHI to patients is allowed under HIPAA in the limited circumstance where the provider: (1) warns the patient that the risk of unauthorized disclosure exists; (2) obtains the patient’s consent to communicate by text anyway; (3) documents the patient’s consent; and (4) offers the patient an opt-out option.
So how do you send automated text reminders? Doing so requires getting permission and setting the right reminder cadence in your system.
- Acquire and document permission from patients
- Set a cadence to send an automated confirmation text as soon as a patient books an appointment, and then send a reminder 2 to 5 days before the appointment
- Use an automated patient text messaging system designed for medical practices to send messages — make sure to choose one that integrates with your scheduling system
Automate patient emails
Automated reminder emails for appointments are another option, and many providers use both text and email. CAN-SPAM laws limit what you can do: you need consent and a bulletproof way to track opt-outs — or risk fines of up to $50,000 per violation.
Email gives you a bit more space and options than text: you can insert your practice logo, office address, and phone number. You can also use friendlier language if you’re trying to present a warm brand.
Providers who use a digital care management platform (software that helps guide patients with customized education paths about their conditions) can include a link. These platforms can improve patient outcomes and help you track patient compliance.
Many providers use email and text for automated patient reminders. Using both increases the chance your patient will review the reminder. For instance, office workers often read email at their computers, which can make it easier to open their calendar and confirm scheduling.
Choose an automated appointment reminder system
Consider the following requirements when choosing automated appointment reminder software:
- Does it interact with your online scheduling system?
- Does it support SMS, email, and phone calls?
- Does it support HIPAA compliance?
A final consideration: Scheduling emails aren’t the only electronic communication you’ll send. Select a system that also supports payment reminders, links to convenient payment options, patient balances, and other communications. Standardized communications (similar look and feel, messages coming from the same source) builds confidence in patients and makes it easier to manage consent and opt-outs.
Manage patient no-shows and rescheduled appointments
While automated confirmations and reminders cut down on missed appointments, there are valid — and not-so-valid — reasons for patients to reschedule, turn up late, or miss appointments. While patients say they rarely miss appointments, 44% reported canceling in the last year, and 15% did without notifying their provider.
Our survey showed the top reasons why patients miss appointments:
- Work conflict (36%)
- Not feeling well enough (33%)
- Transportation (29%)
- Personal emergency (25%)
- Family emergency (22%)
- Feeling anxiety/stress about the appointment (16%)
No-shows not only contribute to inefficiency in your practice, but also can cause delays in patients getting needed medical care.
While you can use late fees and no-show policies with penalties, think carefully about how to roll these out with patients. Discouraging patient no-shows and late cancellation is a delicate dance for providers: warnings and fees can alienate patients. And it’s worth remembering that providers also have to cancel on occasion. Compassionate no-show policies can prevent hard feelings when providers are late or cancel appointments.
In our 2023 survey, medical providers shared the top ways they manage no-shows: use automated reminders (79%); offer more same-day or next-day appointments (54%); and overbook patients (49%).
Some providers offer a discount for prepaying for an appointment — in our survey, 64% of patients said doing so would make them more likely to show up. Many payer contracts prohibit discounts, so check to see if they’re allowed.
Most patients report there’s nothing their provider could do to prevent them from canceling, rescheduling, or not showing up. But the ones who think their provider can influence them say:
- Offer more same-day or next-day appointments (71%)
- See patients on time (57%)
- Send more reminders (40%)
- Require copay in advance (16%)
Many providers take multiple routes to minimize no-shows and late cancellations, such as reminders, simple rescheduling options, and fees or termination. One practice managed a group of frequent cancelers with an innovative probation system that helped cut down on no-shows.
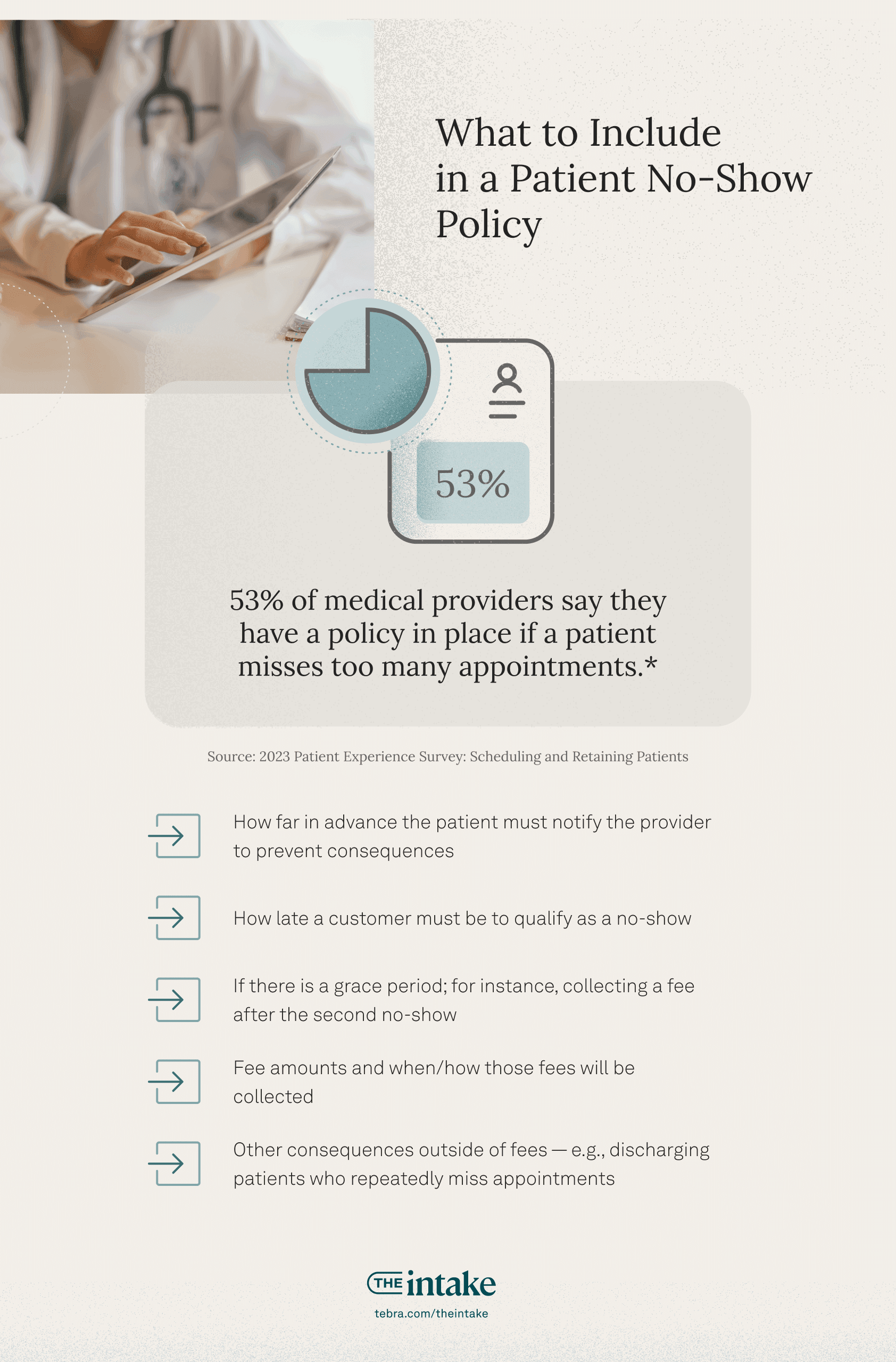
Write and share your patient no-show policy
Providers who take punitive measures to discourage no-shows should publish their policy.
Patient no-show policies should be simple and direct. Overly strict policies can alienate patients. Consider including:
- How far in advance the patient must notify the provider to prevent consequences
- How late a patient must be to qualify as a no-show
- If there is a grace period, for instance, a fee will be collected after the second no-show
- Fee amounts and when/how you will collect those fees
- Other consequences if not a fee, e.g., discharging patients who repeatedly miss appointments
Many practices include the policy and ask for a signed acknowledgment as part of the intake process.
Patient vs. doctor cancellations
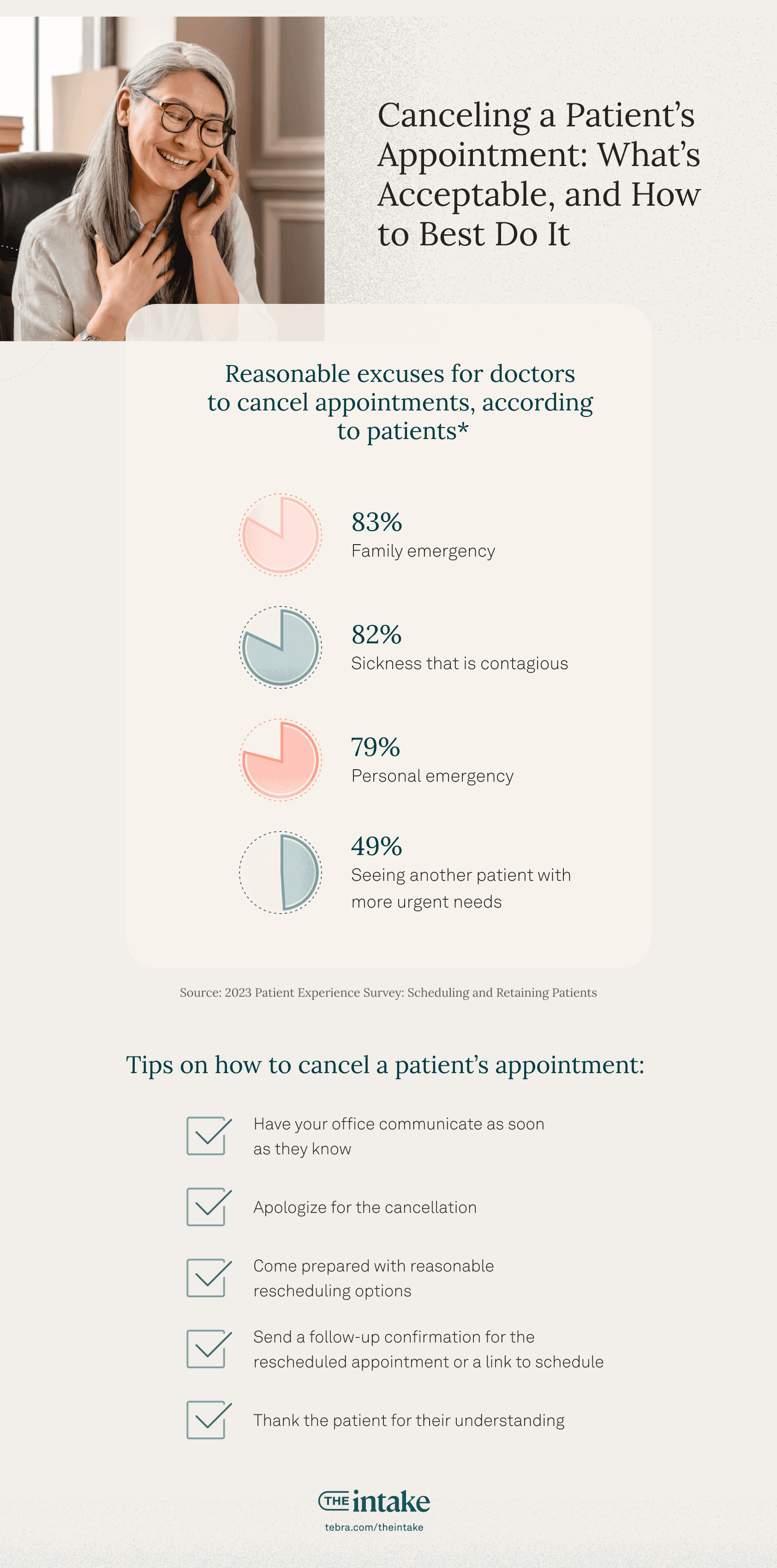
Most patients understand that medical providers sometimes need to cancel appointments. In our 2023 survey, 83% answered yes when asked if it’s ever reasonable for a doctor to cancel or reschedule an appointment.
They had opinions about why you reschedule, though. It may be helpful to know patients picked these as the most reasonable excuses for canceling:
- Family emergency (83%)
- Sickness that is contagious (82%)
- Personal emergency (79%)
- Seeing another patient with more urgent needs (49%)
- Other (3%)
Here are some tips on how to cancel a patient’s appointment:
- Have your office communicate as soon as possible
- Apologize for the cancellation
- Come prepared with reasonable rescheduling options
- Send a follow-up confirmation for the rescheduled appointment or a link to schedule
- Thank the patient for their understanding
Canceling an appointment when a patient is already in the office is especially sensitive, as they’ve invested time and effort to be there. Give them priority in rescheduling and offer immediate or near-immediate alternatives.
What and when not to bill patients who miss appointments
Billing patients for missed appointments can deter no-shows and late cancellations, but there are some things to consider. Our 2023 Patient Perspectives report showed over half of patients would consider switching providers for a better no-show policy. Also, some payer contracts have special provisions constraining when and if you can charge patients for missed appointments. Medicare allows you to charge patients if your policy is consistent with non-Medicare patients, while Medicaid does not allow you to charge patients. Bear in mind payers won’t cover cancellation fees — you have to charge patients.
The AMA advises that it’s acceptable to bill patients for reasonable costs related to cancellations or cancelations within 24 hours if patients are advised in advance.
But it’s not all about legalities. Sometimes preserving the provider/patient relationship — or your online reputation — means not charging fees. Especially consider waiving fees or offering telehealth for patients who are contagious or have family or work emergencies.
The termination letter: Discharging patients for repeated no-shows
The patient termination letter for no-shows is a nuclear option for repeat offenders. Doctors need to provide ample notice and proper documentation to avoid abandonment claims.
You should send a patient dismissal letter for missed appointments at least 30 days prior to termination, and include the reason for dismissal. In addition, include a note about whether and under what conditions a patient could get a second chance with your practice.
Driving more visits from your current patients through communication
Keeping patients engaged with their healthcare — and keeping your practice top of mind — hinge on great communication.
There are 3 types of patient communication in medical practices:
- Doctor-patient (or provider-patient) communication in clinical encounters
- Post-visit communication about treatment plans and follow-ups
- Engagement communications, like newsletters, mass communications about things like vaccines, and even birthday messages
How to improve patient communication
Our polling shows what 50% of patients want most from their healthcare provider is for you to be “a good listener.” 55% want a provider who responds promptly to questions or concerns.
The AMA gives these tips for improving doctor-patient communication:
- Build rapport
- Ask a variety of questions to understand more about their health and habits
- Give lots of positive feedback to round out when you have to deliver constructive feedback
- Ask patients for their feedback
- Express empathy through verbal and non-verbal clues
- Collaborate with patients on their care to encourage adherence
- Use technology to enhance doctor-patient or provider-patient communication but choose carefully — don’t inundate patients with messages
A guide to the patient recall process
It’s always best to schedule a patient before they leave the office, even for an appointment a year in advance, but it doesn’t always happen. Patient recall — or reminding patients to schedule routine checkups or care follow-up visits — is critical to helping busy patients stay on top of their health. And it’s also a way to keep a steady flow of patients coming into your practice.
Patient recalls can be a huge source of consistent revenue. Sending out recall letters will typically mean an increased patient return of 10-20% when issued to an active patient pool. If that recall letter reaches 1,000 patients, that’s 100-200 new appointments — which can be well worth the effort.
Identify key groups that are a good fit for recalls. This might be women due for annual exams, well-baby checks, diabetes patients, patients with chronic conditions, and patients who need annual vaccines like flu shots. Set up a system to run reports on these patients each month from your EHR. Use those reports to reach out to patients to schedule preventive care appointments. The addition of a good practice marketing platform that allows you to automate some of this can be a big time saver. It can also allow you to offer patients the option to get reminders and recalls via text as well as via phone or email.
The patient recall process has 3 components:
- Identify segments that are good fits for recall campaigns. You can run monthly reports in your EHR, and preferably you have a practice growth automation platform that can automate these messages.
- Communicate with patients. Common methods include postcards, calls, texts, or emails (and sometimes a combination). According to a Twilio survey of 2,500 consumers, 86% of people prefer businesses contact them by email, unless the message is urgent — then people prefer text 2.5 times over email. Practices have had success with patient recall message campaigns for important medical needs like vaccines or outstanding follow-up appointments.
- Schedule appointments. Besides being cheaper to deliver, electronic communications like text and email have a big advantage: You can put self-service scheduling links in the message.
In addition to routine patient recall messages, you can also review your electronic health records (EHR) to catch older missed appointments and run large-scale campaigns to try to get some of those patients to return. Planning these campaigns a few weeks before seasonal slowdowns can even out your calendar and bring business in.
Patient follow-ups increase return visits
Follow-up messages can help engage patients and remind them to schedule follow-up appointments. Many practices print out a summary of the patient encounter, including the next appointment. But that doesn’t mean you can’t reach out after. Post-appointment check-ins can include summaries of the appointment, thank you messages for visiting the office, reminders about scheduling, and a scheduling link.
In our recent survey, medical providers shared their most common methods of following up:
- Phone call from staff (78%)
- Patient portal (58%)
- Automated calling system (28%)
Some patients may be skeptical about the necessity of routine check-ups. Address this by educating them during their visit. Front-office staff can brief patients before they leave, or targeted newsletters can emphasize the value of regular appointments.
How experience and engagement can drive patient loyalty
In the Amazon era of one-click convenience, patient loyalty is harder to maintain. Busy patients often seek more convenient experiences: self-service scheduling, fast appointment availability, digital payments, and so on. They may also feel less loyalty to clinicians who have to spend more time in EHRs and less time with patients than in the past.
But independent medical practices interested in building patient loyalty have better tools today:
- Save time for patients by using EHRs and related systems that remove redundant clicks and offer AI note-taking
- More easily provide convenient self-service scheduling, automated text reminders, and simple payment options (as well as payment plans and subscription-based services)
- Email systems and other tools for engaging patients
- Automated feedback solicitation to improve the patient experience
A survey by NRC Health showed more than 80% of patients would switch providers for convenience.
Patient engagement leads to better outcomes
Patient engagement means developing a partnership in healthcare. The most effective providers make patients feel their healthcare matters to everyone in the practice, including the full care team and office staff.
The perception of care and empathy goes a long way to instilling loyalty and influencing patients to take actions that improve their health outcomes.
A true healthcare partnership is not just about what the outcome is, but whether the best course of action was taken under the circumstances. In other words, patients want to know if you’re giving the same advice you’d give to your family.
Patient engagement is key to healthy patients and a healthy practice. Numerous studies show engaged patients with chronic diseases live longer, and patients who attend their follow-up visits on time are good for your practice.
This means delivering optimal healthcare outcomes isn’t just about the quality of clinical care. Making it easy and pleasant for patients to work with your practice makes it more likely that they will schedule follow-up treatments, ask questions, and collaborate on their health goals.
Excellent communication is a key factor in engagement. Digital tools make engaging patients easier, by automating personalized communications and allowing you to communicate asynchronously via channels like text messages, social media, and patient portals. Better-designed EHRs can also remove tasks from providers’ plates, freeing up time for active listening.
The end-to-end patient experience also matters. Unpleasant experiences can shut down engagement, and pleasant, convenient ones can increase it. Patients who can easily book and reschedule appointments, make payments, have positive experiences with your practice, and receive helpful communications will be easier to engage.
Digital patient engagement
Digital patient engagement can mean many things: interacting with patients (and potential patients) on social media, sending newsletters and other informative emails, and using a patient portal to help patients access their test results and treatment plan.
The key is communication: you want patients to feel confident that they haven’t missed anything. And periodically checking in keeps you top of mind and often reminds patients to schedule that next appointment.
Personalizing the patient experience and management: Care, education, and billing
Relationships are key in getting the best outcomes in medical care. But with busy providers seeing lots of patients, you may have a hard time getting to know yours. An EHR helps you deliver personalized patient care. If you take notes (or have AI do it), you can refresh yourself on the details of a patient’s situation and preferences before they arrive.
And it’s vital that you don’t just hand off an assessment, especially if it includes words that scare patients, like suspicious, insufficiency, failure, or malignancy. You need to explain anything you’ll include in your patient summary to avoid alarming or confusing patients.
Personalized patient experience tools can also be a huge support to patients. If you have an automation platform, you can provide the full range of personalized patient communications: follow-up visits, prescription refills, and bill payment.
How a positive patient relationship can drive return visits
A strong doctor-patient bond is more than just a hallmark of quality care; it’s a cornerstone of patient retention. In an era where healthcare is ever more attuned to consumer desires, patients want more than just a medical appointment. They seek seamless digital interactions, such as emailing or texting their provider, or direct communication via a portal.
Independent practices are well-positioned to achieve this. You can offer the personalized care patients crave, serve as their health coach and cheerleader, and seamlessly integrate follow-ups into their treatment plans.
On the other hand, some factors will harm relationships. Long wait times, lack of follow-ups, and poor communication make patients feel undervalued and anonymous.
Regular, personalized communication can drive satisfaction and return visits. For instance, patient recall campaigns, which target those overdue for annual exams or follow-ups, benefit both the provider and the patient by reinforcing the bond and encouraging preventive care.
Tips and timesavers that make active listening in healthcare easier
One of the hardest arts in medical care is obtaining a good patient history. If a provider isn’t attuned to cues and asking open-ended questions to elicit lots of detail, patients may omit information they consider irrelevant or embarrassing.
But that’s hard when providers are stretched for time. A 2018 study published in JAMA found the average clinician interrupts a patient just 11 seconds into the encounter, and inquired about a patient’s agenda only 60% of the time.
The complexity of running a practice and the challenge of patient volume can have deep impacts on time and focus.
For many healthcare providers, time spent in clinical systems and administrative tasks is the greatest obstacle to active listening. Poorly designed EHR systems are the culprit for many: studies report that the average physician spends twice as much time with EHRs as with patients, in addition to personal time off hours. It’s crucial to choose an EHR designed for usability; AMA research found it saves time and reduces burnout.
Using the same operating system for clinical and administrative tasks can also save time for active listening in healthcare. A way to be a more active listener is to ask patients open-ended and follow-up questions, such as:
- What brings you here today?
- Is this a new problem?
- When does this bother you the most/what triggers it?
Ways to keep patients happy (and loyal)
The factors that make for happy patients are:
- Excellent clinical care
- Positive interactions with practice staff
- A pleasant, clean, and caring practice
- Convenient location and interactions
Digitally driven convenience is probably the easiest and most important place to invest — and it also benefits staff, who then have more time for patients. Self-service tools for patient intake and scheduling, as well as automation, like patient reminders, save staff lots of time.
Many of those same tools offer convenience that keeps patients happy. Patients prefer self-service scheduling over talking to your practice, so it’s a win-win. Same for things like automated payments (convenient text/email payment reminders with payment links embedded) and appointment reminders.
Improve patient wait times
Patient wait times also impact their satisfaction and likelihood of returning to your practice. One unusual way to improve patient wait times: automated reminders and easy, 24/7 options for rescheduling can decrease patient no-show rates — so practices can cut down on double-booked appointments.
But there are lots of ways to make wait times more pleasant:
- Allow patients who are ill or fear contracting illness from a waiting room to use text messaging and contact-free check-ins from their vehicle
- Offer different seating options: seats facing a TV, quieter areas for professionals who are working, and a kids area
- Provide free WiFi, reading materials, drinks, and other pleasantries
- Keep patients updated about longer wait times
One practice told us they popped popcorn or used a small oven to bake homemade cookies on the busiest afternoons. Patients loved the treats and the delightful way the office smelled.
Finally, waiting time isn’t just about the time before an appointment. A doctor shared that one of the biggest complaints he heard was that it took too long to receive paperwork after the visit. Also, consider the convenience factor for any tests: can they get X-rays or other diagnostic the same day in a nearby location? This convenience saves time.
Make the most of time with patients
One thing patients value: time with their providers. While you can’t make more time in a day, you can use automation to improve your ability to spend time with patients. The single biggest time-saver for medical practices is applying automation to as many places as possible. Having integrated systems for billing and EHR (for instance) may eliminate having to enter information multiple times. Robotic process automation bots can be programmed for manual tasks.
Building effective patient retention programs
Retention can positively impact practice success.
Many patient retention drivers boil down to care, convenience, and staff interactions, but there are many levers to pull. Patient retention strategies range from investing in your brand to discounts, payment flexibility, and membership programs.
How to calculate and use your patient retention rate to increase visits
The patient retention rate is a key metric in practice performance. Tracking and understanding retention and churn is critical for evaluating retention investments, and it’s a critical indicator of performance growth or decline to come.
A common patient retention rate formula measures on a yearly basis or you can do it on a rolling basis (like a monthly retention rate, or measuring the previous 12 months at any point in the year).
Here’s the year-over-year formula:
- Subtract new patients from total patients this year
- Divide the total by the number of patients you saw last year
So if you had 1,200 patients this year, 300 of which were new, and you had 1,150 patients last year, you’d have a 78% patient retention rate.
Patient rewards programs support retention
Patients spend a lot of money on healthcare, and they appreciate getting some of it back. Some independent practices support the patient relationship with things like billing credits for referring patients. Patient reward programs might also include getting points and merchandise or discounts for completing health goals.
Over half of patients in our recent survey have referred another patient, and many providers capitalize on this by instituting patient referral reward programs. These programs offer a dual benefit: patients feel appreciated and you receive more referrals.
40% of providers in our survey say they can attribute up to 25% of their new patients to referrals. Another 26% say they can attribute up to between 25%-50% of new patients to referrals. Having a patient referral reward program can help you boost patient acquisition.
Tracking referrals and rewards might be a challenge for your staff. One tip about asking for patient referrals: many searches lead to the wrong result. Make sure all your business profiles feature full and correct information about your practice.
Robust patient scheduling and retention drive healthy practices
The right technology can improve convenience, care, and quality interactions. The kind that makes it easier for patients to interact with your practice at their convenience, and effortless technology supports that free up providers’ and admin staffs’ days to focus on patient interactions.
Visit our Patient Experience page to find out more about how integrated, intuitive practice software can make it easier to keep your calendar full and your patients healthy.
You might also be interested in
Tackling patient no-shows and cancellations. Download this free report to learn how to stop patients from skipping and canceling their appointments and how to deal with persistent no-shows.
How to get patients to keep coming back. Learn what influences patient choices and behaviors in the 2023 Patient Perspectives report.