Staying ahead of the curve: Medical billing industry trends to watch
Learn what the future holds for the medical billing industry in Tebra’s industry benchmark report.

Most Popular
At a Glance
-
- For established and start-up medical billing companies looking to grow, there are many opportunities to boost revenue.
-
- Ensuring clear communication and transparency with medical practices can lead to referrals.
-
- Offering more than one core billing service can help to diversify income.
-
- Leverage payment collection as an opportunity rather than a challenge.
Between inflation, supply chain shortages, and a pandemic, just about everything around the American economy has changed — and medical billing companies aren’t immune from disruption or innovation.
The difference is that a medical billing service can still thrive in this period of economic uncertainty. The pandemic, in fact, rapidly shifted how healthcare works in the United States and highlighted the value of hiring a medical billing company for many providers.
The future of US medical billing is largely optimistic, and in our medical billing benchmark report, we found out why.
The current state of medical billing in the United States
If we wanted to describe the state of US medical billing briefly, metamorphosis might be the ideal term. The industry is not just changing but rapidly evolving. With healthcare providers dealing with labor shortages and mounting expenses, these circumstances may prompt office managers to outsource one of their most time-consuming tasks — medical billing.
Yet, a medical practice requires more than a core medical billing service to succeed, and many billing services are diversifying their offerings in response.
Today, medical billing companies may offer an array of services, including:
- Claims submissions
- Claims follow-up
- Appeals
- Patient support
- Medical coding
- Working old A/R
- Verification of benefits
- Telehealth billing
Many medical billing companies also include add-on services, like:
- Chart audits
- Practice technology support
- Credentialing
- Payer contract negotiations
- Compliance consulting
- Practice marketing
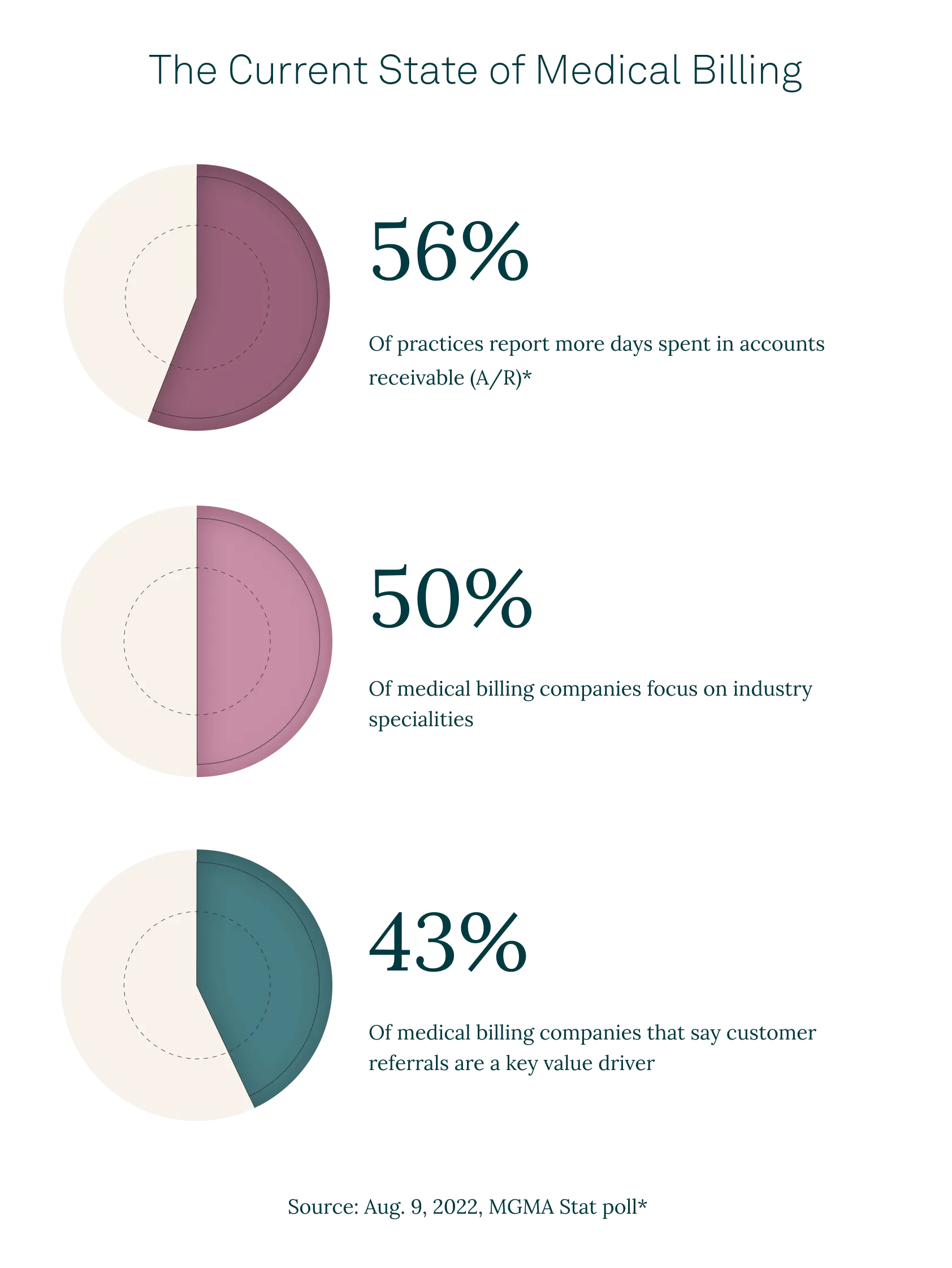
Based on our industry research, half of all US medical billing services are highly specialized, with the top 3 niches centering around mental health, physical therapy, and family practice. Most organizations work across state lines, although 1 out of 10 companies will not process medical practice claims from California or Texas.
“While the industry offers a bright outlook, ensuring continued profitability remains a core focus of most companies.”
While the industry offers a bright outlook, ensuring continued profitability remains a core focus of most companies. As a result, 40% of medical billing companies require a minimum invoice amount before taking on new customers, in addition to other potential requirements, according to our research.
In terms of pricing, percentage-basis billing dominates as the most popular model. But billing companies continue to use claims-based and hourly charges, too.
Still, no other metric has changed and challenged the industry as drastically as technology.
The impact of technology on the industry
Covid-19 resulted in an overall spike in demand for digital medical billing services, but despite the multiple benefits of digitization and automation, few medical practices have adopted new systems and processes. From EHR systems to managing their online reputations, medical billing companies and their clients are facing a new world of business.
“Often, a medical practice does not have the bandwidth to train staff on new medical billing technology.”
There are 2 primary reasons for the lag, namely the closure and acquisition of private practices by larger enterprises, and outsourcing. Often, a medical practice does not have the bandwidth to train staff on new medical billing technology, even if they have the funds to invest in modern practice management solutions. This scenario provides medical billing companies with an opportunity to better serve their healthcare organizations and attract new customers.
Still, many billing companies are also catching up to innovation.
As of 2023, less than one-third of medical billing companies used artificial intelligence (AI) automation, robotic process automation (RPA), Health Level 7 (HL7) integrations, and outsourcing to manage workflows, according to our industry research. As a result, nearly half of medical billing companies in our study have cobbled together 2 or 3 different systems to complete their billing services.
Technology, however, may prove to be the answer to many challenges facing medical billing professionals today.
What challenges do medical billing companies face?
According to our research, increased competition and fewer customers are the overarching challenges for medical billing companies. Requirements for new billing customers (such as minimum number of monthly claims and invoice amounts) also cut out many start-up clinics and practices, further reducing the customer pool. In addition, inflation and skyrocketing costs of high-deductible health plans negatively patient affect spending, either from fewer patients or difficult collections.
Our research found that patient balances can represent up to 20% of receivables. Additionally, 38% of medical billing companies say that they are finding it difficult to collect at the time of service, and 27% don’t have proper insurance for patients on file. Only large billing companies have high collection rates of 11% to 20%.
“For a competitive edge, medical billing companies need a way to streamline cash flow, tap into new customer bases, and reduce collection time.”
One study found that 25% of adults are skipping care or medicine due to rising costs. Many may also pay bills late. This mirrors a drastic increase in time spent in A/R in 2022 for 56% of practices.
At the same time, 70% of US medical billing companies have increased operational spending since 2022. Keeping up with the latest medical billing software and expanding services requires working capital upfront. Billers must balance patient payment collections, regularly evolving compliance requirements, and industry standards to stay in the game.
For a competitive edge, medical billing companies need a way to streamline cash flow, tap into new customer bases, and reduce collection time. And ideally, these efforts will dovetail into cost-effective operational spending.
How can you stay ahead of the curve in the medical billing industry?
The research shows that high-growth medical billing companies, defined as businesses with 2 years of year-on-year revenue growth of 11% or more, have a few key characteristics.
Offering additional services may be a route to expansion. According to our survey, 91% of these companies offer appeals services. Other potential services to consider are:
- Practice technology consulting and support
- Credentialing
- Compliance consulting
- Marketing
These services branch out beyond billing, allowing medical companies to diversify, retain, and attract new clients. Many practices and medical providers are exhausted from juggling various technology and service vendors. Giving them a “one-stop-shop” or providing them with additional services can also build a stronger customer relationship while generating revenue.
“52% of high-growth companies use robotic process automation (RPA), and 29% use patient collections automation.”
Another key finding is that 52% of high-growth companies use robotic process automation (RPA), and 29% use patient collections automation. In other words, implementing technological solutions, such as RPA, e-billing, and e-payments may unlock growth opportunities for medium-sized and smaller firms.
What are the factors driving the US medical billing outsourcing market?
According to a study from Acumen Research, North America outsources the most medical billing services and accounts for 46.8% of the medical billing outsourcing market. The market size was estimated to grow at a CAGR of 11.3% from 2022 to 2023. Our own study highlights that 7 out of 10 medical billing companies feel positive or very positive about outsourcing in the industry.
There are many factors contributing to the rising success of medical billing outsourcing in the United States. Providers continue to see outsourcing as an opportunity to reduce costs and fuel growth. Employing outsourced medical billers allows a healthcare provider to tap into the latest medical billing software, limit staffing needs, and potentially reduce costs.
Billing service organizations can leverage these benefits to attract and retain more customers going forward.
What are the best practices for medical billing companies today?
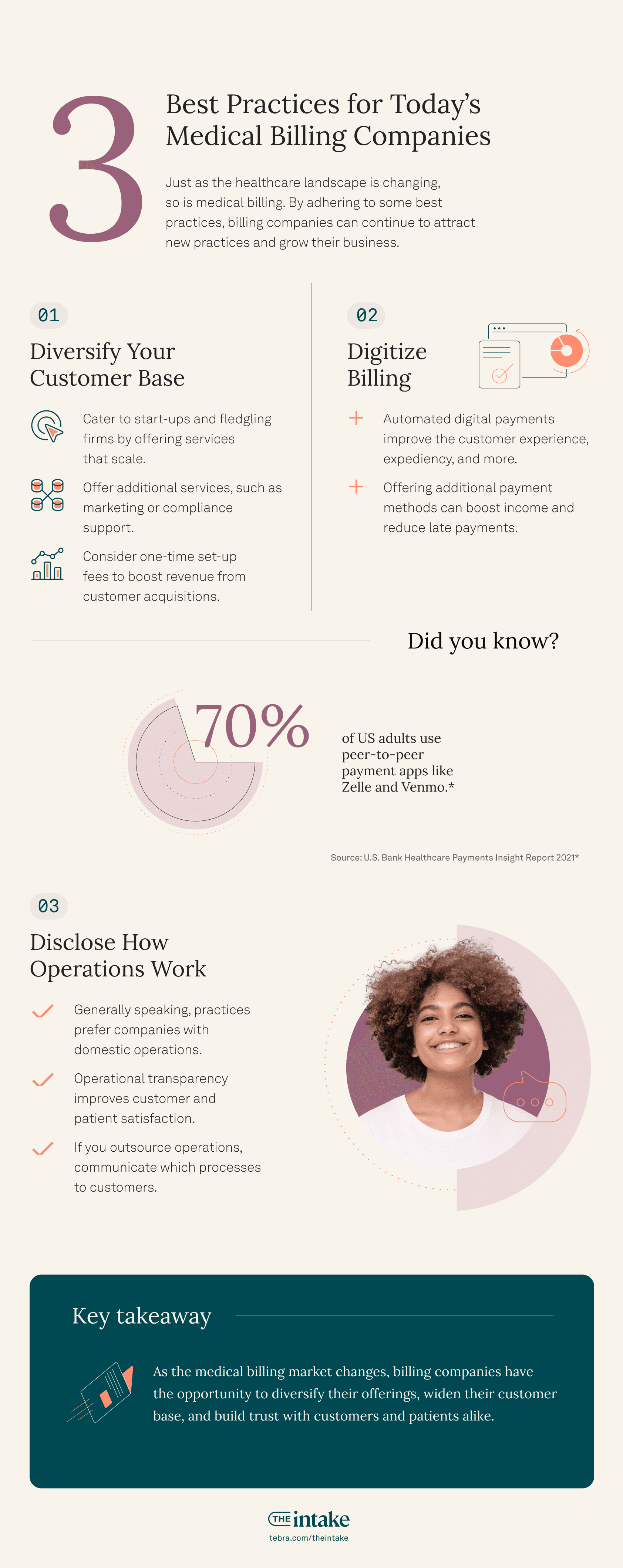
Best practices and trends today for medical billing companies fall under 3 main categories: diversification, digitization, and disclosure.
Diversifying your customer base
The closure of many independent practices post-Covid highlights the importance of customer diversification. Even for niche medical billing companies, it’s critical to have a larger customer base. Offering additional services, such as marketing or compliance support, can both increase revenue from existing customers and attract new ones.
“An untapped source of revenue for many billing companies is start-up practices.”
Another untapped source of revenue for many billing companies is start-up practices. New or fledgling firms rarely have the required revenue or monthly invoice amount to qualify for full services. Medical billing organizations can remedy this by providing smaller start-up packages or services that scale as the company grows.
Yet, it’s also important to be proactive and realistic when setting rates. In addition to potential revenue or invoice minimums, most medical billing companies use a combination of one-time set-up fees to cover upfront expenses and ongoing fees.
Digitizing billing
Automating the billing process provides several benefits, including:
- Improved customer experience
- Faster payments and processing
- Easier collections
- More transparent accounts
- Clearer communication between front and back offices
It’s not just billing companies or providers that benefit from digitizing healthcare. Patients are demanding it, too. A study from U.S. Bank found that people prefer digital options for bills, including P2P (peer-to-peer) payment options like PayPal or Zelle.
Patients have already experienced the freedom, flexibility, and convenience of making bill payments with other essential services. So, why not with healthcare? Patients expressed in another survey that they would use more digital or mobile wallets to pay if given the option of mobile healthcare payment in the same way that they pay any other bill.
“For medical billing companies and providers, offering additional payment methods can boost income and reduce late payments.”
“An integrated EHR, billing, and communications platform lets patients store a credit card securely in its system and then pay bills with a single click. Patients benefit from the convenience of taking care of obligations any time, wherever they may be, without having to find their checkbook and a stamp,” says Kevin Clinton, Director of Marketing, Payment Solutions at Tebra.
For medical billing companies and providers, offering additional payment methods can boost income and reduce late payments. Streamlining the payment process makes it easier for patients to pay immediately or enroll in auto-payments for recurring visits. At the same time, the back office staff doesn’t need to review every single account, only the ones that stand out.
Operational transparency through disclosures
One of the best ways to form the foundation of a satisfied client relationship is to be completely transparent about operations. A sound example of where this matters is whether or not your operations take place in the States or abroad. While most medical billing providers outsource some aspect of their work overseas, providers like their billing company to be located locally.
“Data has consistently shown that medical practices strongly prefer a billing company with all operations within the United States. More often than not, it’s due to the practice previously working with a medical billing company that offshored its operations, and they experienced poor communication or performance,” says Jamie Howard, Channel Sales Manager at Tebra.
“One of the best ways to form the foundation of a satisfied client relationship is to be completely transparent about operations.”
If you do outsource aspects of your services (or all of them), communication is key. Disclosing your processes, how your billing system works with their EHR platform, and realistic support response times will build trust.
This trust is critical since 43% of medical billing companies say customer referrals are the key value driver when they win new business, and 82% say word-of-mouth is their marketing priority for the next year, according to our industry research.
If you are transparent with your customers, not only will they stay longer, but they will also bring business to your company.
You Might Also Be Interested In
Medical billing company best practices: Learn why diversifying, digitizing, and operational transparency are your keys to growth in our benchmark report.
Stay Ahead with Expert Healthcare & Billing Insights
Get the latest industry updates, financial tips, and expert strategies — delivered straight to your inbox.

Suggested for you
Stay Ahead with Expert Healthcare & Billing Insights
Get the latest industry updates, financial tips, and expert strategies — delivered straight to your inbox.











