Overview
- Efficient revenue cycle management improves cash flow and reimbursements.
- Automating billing processes reduces errors and administrative burdens.
- Monitoring KPIs helps optimize financial performance.
Unlike many other industries, healthcare requires a multistep, retrospective payment process. Healthcare providers render a service and often don’t receive reimbursement for weeks — or even months. The process by which providers are paid, known as revenue cycle management (RCM), only goes smoothly when those providers prioritize people, policies, and technology in the following ways:
- Employ highly skilled medical billing and medical coding staff who understand complicated payer requirements.
- Draft clear and concise RCM policies and procedures.
- Leverage RCM technology and analytics to promote revenue integrity, improve charge capture, and increase patient engagement.
It’s a tall order, and many healthcare organizations — including health systems and independent practices — struggle with one or more of the RCM strategies listed above.
In this article, we’ll dive into this pressing question: what exactly is healthcare’s revenue cycle? We’ll provide revenue cycle management steps and outline the benefits of revenue cycle management. Finally, we’ll discuss how to improve revenue cycle management to help healthcare providers promote financial sustainability.
What does RCM stand for in healthcare?
Healthcare revenue cycle management (RCM) is an umbrella term for the multistep process healthcare providers use to identify, manage, and collect revenue. Healthcare revenue cycle management begins the moment a patient schedules an appointment and ends when the provider collects all the reimbursement to which they’re entitled. This includes any amount insurance companies and patients owe.
“Healthcare revenue cycle management begins the moment a patient schedules an appointment and ends when the provider collects all the reimbursement to which they’re entitled.”
Over time and with the rise of high-deductible health plans (HDHPs), patients are increasingly responsible for a larger portion of their healthcare bills. For example, 29% of covered workers are now enrolled in a HDHP. Some sources estimate this number is well above 30%.
This means that if healthcare providers want to improve revenue cycle management, they must engage patients and improve patient payments. Patient engagement directly benefits revenue cycle management. In fact, it’s safe to say that there is no healthcare revenue cycle management without patient engagement.
Pro tip: To improve healthcare revenue cycle management, focus on patient engagement. As patients’ financial responsibility continues to increase, providers must engage insurance companies and patients equally.
What are some of the biggest healthcare revenue cycle management challenges?
For today’s healthcare providers, revenue cycle management challenges happen every day. Here are some of the most significant ones to emerge over the last few years:
Decreased reimbursement from insurance companies
In its calendar year 2024 Physician Fee Schedule Final Rule, Medicare finalized a 3.4% payment cut. It’s not surprising that 38% of physicians say the financial state of their medical practice has worsened, with only 60% meeting their revenue goals. Across the board, healthcare providers haven’t been able to keep up with inflation. Medical practices need a plan to offset this decrease and improve revenue cycle management. Together, effective RCM processes and analytics promote financial sustainability.
Healthcare disruptors
Nontraditional, lower cost, and easier-to-access healthcare disruptors make it harder for independent providers to attract and retain patients and maintain a steady revenue stream. Practices need to engage patients proactively even before they schedule an appointment by focusing on search engine marketing, advertising, and social media. Standing out from competitors directly benefits revenue cycle management.
Increased patient financial responsibility
More cost-sharing arrangements between patients and insurance companies make it harder for to collect patient payments. Practices must focus on transparent prices and leverage technology that makes it easy for patients to pay.
Insurance complexities
The complexity of the insurance system makes it challenging to get paid correctly and on time. Medical codes and billing requirements change frequently. Across HealthCare.gov insurers with complete data, nearly 17% of in-network claims were denied in 2021. Insurer denial rates varied widely around this average, ranging from 2% to 49%.
Shifting payment models
The shift from fee-for-service to value-based payments creates economic uncertainties that make it difficult to predict risk and forecast revenue. Medical practices need RCM analytics to make informed business decisions.
Staffing shortages
Difficulty recruiting and retaining revenue cycle management staff not only drives up costs, but also has consequences for compliance and cash flow. For example, nearly all respondents to a recent survey said healthcare staffing shortages continue to negatively impact revenue cycle management and patient engagement.
These same staffing shortages also affect insurance company reimbursement, patient payments, and the patient experience. In 2022, front office staff experienced a 40% turnover rate, with clinical support and business operations support staff turnover rates close behind at 33%.
“Nearly all respondents to a recent survey said healthcare staffing shortages continue to negatively impact revenue cycle management and patient engagement. ”
Being short-staffed impacts healthcare revenue cycle management. In 2022, 56% of medical groups reported that their time in accounts receivable (A/R) increased, often due to staffing difficulties. In addition, short-staffed billing departments may need more resources to manage claim denials.
Why is healthcare revenue cycle management important?
Revenue cycle management — particularly medical billing and medical coding — is important because it helps providers get paid under fee-for-service and value-based payment models.
Revenue cycle management imposes structure on an otherwise complicated process vulnerable to errors and omissions. It ensures healthcare providers have the right staff, practice management policies and procedures, and charge capture technology in place for efficient claims processing and revenue integrity.
Without revenue cycle management, healthcare providers may leave money on the table or risk denials, recoupments, and fines.
What are the benefits of healthcare revenue cycle management?
Some benefits of revenue cycle management include the following:
- Enhanced charge capture for revenue integrity
- Cleaner claims
- Improved medical coding and medical billing efficiency
- More reliable RCM analytics for strategic business decisions
- Positive insurance company relations
- A smooth patient financial experience that enhances patient retention
- Steady cash flow
Effective revenue cycle management ultimately helps medical practices focus on what’s most important: high-quality patient care.
“Effective revenue cycle management ultimately helps medical practices focus on what’s most important: high-quality patient care.”
Smooth revenue cycle management puts everyone’s minds at ease knowing that services rendered will be reimbursed correctly and on time. This is especially important for independent practices. Cash flow is critical for investing in new technology, marketing the business, paying salaries, covering overhead, and more.
What are the revenue cycle management steps?
While the specifics vary by practice size and specialty, the basic 10 RCM steps are the same:
- Patient scheduling and registration. Providers collect demographic and insurance information.
- Pro tip: Patient-completed digital intake forms reduce errors.
- Eligibility verification and prior authorization. Staff verify coverage and obtain any necessary prior authorizations from insurance companies.
- Patient visit and care delivery. Providers deliver care.
- Clinical documentation. Providers document details such as the patient’s history, exam, and medical decision-making, as well as treatment plan and medical necessity. They increasingly document details related to social determinants of health to promote health equity and value-based care.
- Pro tip: Develop tip sheets or electronic health record (EHR) templates with up-to-date medical codes.
- Coding. Medical coders and billers assign ICD-10-CM, CPT, and HCPCS codes based on clinical documentation.
- Claim submission. Practices submit claims to insurance companies, usually via a clearinghouse that checks for errors.
- Pro tip: Select a clearinghouse that operates nationally, provides online access and real-time support, and explains error codes.
- Payment posting and reconciliation. After insurance companies process a claim, they remit full or partial payment or issue a denial. When payment is rendered, practices reconcile that amount with the anticipated payment to identify and investigate potential underpayments.
- Patient billing. If practices haven’t collected the copayment or coinsurance, they bill patients for any remaining amounts.
- Pro tip: Up-front collections prevent back-end follow-up. Make it easy for patients to pay digitally, promote price transparency, and offer payment plans. Time of service payments also have benefits.
- Denial management. Staff investigate and potentially appeal any denials.
- A/R follow-up. Staff follow up on unpaid balances from insurance companies and patients.
Each of these revenue cycle management steps are critical. That’s because each builds on the step before to result in accurate and timely payment. Devote equal attention to each step for the biggest return on investment.

What individuals in the medical practice are involved in revenue cycle management?
Everyone plays a role in healthcare revenue cycle management. However, the specific steps necessary to gather information, submit claims, and process all payments usually require direct input from:
- Auditors
- Medical billers
- Medical coders
- Patient financial advocates
- Receptionists
- Schedulers
These individuals are considered the revenue cycle management team.
How does healthcare revenue cycle management help with the flow of patient information?
Effective revenue cycle management ensures that patient information flows smoothly to the insurance company for processing and payment. Without revenue cycle management, information would remain siloed within the practice management system.
Collecting information
Technology integration is critical. For example, the first step in RCM (i.e., collecting the patient’s demographic and insurance data) occurs via the patient portal, digital intake form, over the phone, or in person.
This data resides in the practice management system; however, with integration, this information is also easily accessible in the EHR where it’s linked with clinical data. For example, medical codes a physician in the EHR automatically populate a claim in the practice management system. This automation is impossible without integration.
Translating information to medical codes
After the patient encounter, medical coders and billers read clinical documentation and assign accurate, complete, and specific ICD-10-CM, CPT, and HCPCS codes to represent what occurred and why.
Practices may or may not have internal edits in their billing software to identify potential errors and help to ensure clean claims. For example, many internal edits check Medicare local or national coverage determinations, national correct coding initiative edits, medically unlikely edits, and top denial reasons (e.g., upcoding, unbundling, incorrect modifiers, or mismatched codes).
Submitting information to insurance companies
Next, the practice usually submits the electronic medical claim to a clearinghouse. The clearinghouse scrubs the claim and double-checks it for errors. Once it passes inspection, the clearinghouse securely transmits the claim to the insurance company.
Remember: when insurance companies process payment, they only receive the claim — not the entire medical record. (The exception is when they request the record as part of a prepayment process or a post-payment audit.) That’s why medical codes must reflect patient severity, acuity, and services rendered. Omitting codes means the practice could lose money. Adding extra codes could lead to overpayments and recoupments — or to denials.
Once an insurance company receives a claim, it begins claim adjudication. The payer may apply its own edits before paying the claim in full (or part) or denying it entirely.
Insurance companies render payment via electronic funds transfer (EFT). This transaction may include electronic remittance advice (ERA) to convey additional information such as contract agreements, secondary health plans, patient benefit coverage, expected copays and coinsurance, capitation payments, or Internal Revenue Service withholding.
Insurance companies may also use claim adjustment reason codes (CARC) and remittance advice remark codes (RARC) to explain payment adjustments.
Payment reconciliation happens next. Medical billers compare and verify reimbursements with billed charges. They also investigate any discrepancies. For example, they may need to resolve a medical coding error, contractual issue, or technical problem. This is also when practices usually bill patients for the balance of the invoice if they haven’t already collected it.
When there’s a denial, healthcare revenue cycle management promotes root cause analysis and follow-up. This process of information generation, transmission, reconciliation, and ongoing analysis is what makes RCM so important.
Without good RCM, information would not flow from the healthcare provider to the insurance company to enable payment.
How can a healthcare organization improve its revenue cycle?
The best ways to improve revenue cycle management will be different for every practice according to its unique challenges. For example, one practice might struggle with A/R and denial management. Another might struggle with cash flow, patient payments, charge capture, or staff retention.
“The best ways to improve revenue cycle management will be different for every practice according to its unique challenges.”
But there are universal strategies that can help improve healthcare revenue cycle management. These include the following:
- Leverage healthcare revenue cycle management dashboards and customized reports to monitor denials and prevent them proactively.
- Leverage robotic process automation (RPA) to augment staff abilities.
- Pro tip: Here are 5 areas where RPA can help healthcare providers improve revenue cycle management: ERA processing, payment processing, clinical note creation, payment plans, and 835 uploads.
- Outsource healthcare revenue cycle management to improve charge capture, medical coding, medical billing, and revenue integrity.
- Perform frequent medical coding and medical billing audits.
- Prioritize the patient financial experience (e.g., give patients more and easier ways to pay) to enhance patient collections.
- Educate staff about common denials and how to avoid them.
- Stay on top of relevant coding guidelines and medical coding changes.
- Use billing edits to catch errors and omissions before claim submission and ensure smooth claims processing and payment.
- Work all claim denials in a timely manner.
What are the most important healthcare revenue cycle management policies and procedures?
Some of the most important revenue cycle management policies and procedures include the following:
Medical coding, medical billing, and claim submission
Who will assign medical codes, and how? What is the process for charge capture? What workflows will everyone follow to ensure accurate and timely medical claim submission?
Pro tip: To keep the claims submission process running smoothly:
- Maintain dedicated staff to focus on and address claim edits
- Prioritize timely charge capture and enter charges daily
- Submit claims to the clearinghouse daily
- Work claim edits daily
Clinical documentation improvement query process
When questions about clinical documentation arise, who will resolve those questions and how?
Denial management
Who will monitor and manage denials? Will staff prioritize certain ones?
Internal coding guidelines
In addition to official coding guidelines, will staff use any additional guidelines based on feedback from insurance companies or the desire for internal data tracking?
Key performance indicator (KPI) reporting
What KPIs will the medical practice track, and how often? How will it calculate those KPIs? What will it do with the information?
Medical coding and medical billing productivity standards
What are the expectations for coders and billers, and what happens if they don’t meet those expectations?
Patient payments and collections
What will the practice require of patients? For example, will it require up-front collections? If so, how much? What is the process for balance billing the patient or providing refunds when necessary?
Registration and financial screening
What workflows will staff follow to ensure data integrity? Can the practice leverage digital tools that enable patient self-service (e.g., digital intake forms or patient portals)? Will staff offer payment plans or other means of financial assistance when applicable? If so, what criteria will they use to determine whether patients qualify?
What is revenue integrity, and how does revenue cycle management enable it?
Revenue integrity refers to billing and collecting all revenue to which a healthcare organization is entitled. Note that revenue integrity is not synonymous with revenue maximization. That’s because the latter often implies billing and collecting as much as possible without regard for legal and contractual compliance.
The National Association of Healthcare Revenue Integrity (NAHRI) says the goal of revenue integrity is to prevent recurring issues that can cause revenue leakage and/or compliance risks.
Revenue cycle management enables revenue integrity by introducing oversight and a system of checks and balances that mitigates risk and promotes compliance. The combination of skilled staff, policies and procedures, and robust technology pave the way for accurate reimbursement.
Pro tip: For more information about compliance program infrastructure, program adaptations for small and large entities, and other resources, check out the recently updated Office of Inspector General’s General Program Compliance Guidance.
How can healthcare providers achieve revenue integrity?
Here are 3 strategies to achieve revenue integrity in revenue cycle management:
- Audit frequently. Medical coding audits help identify potential revenue cycle errors or omissions. Audits also help inform educational opportunities and workflow improvements.
- Leverage the right technology, including healthcare revenue cycle management analytics. When deployed correctly, the right technology can augment staff’s abilities through built-in claim scrubbers, automated eligibility, denial management tools, and more.
- Promote a culture of compliance. Ensure everyone understands the importance of revenue cycle management and their role in supporting it.
What is the link between healthcare revenue cycle management and financial sustainability?
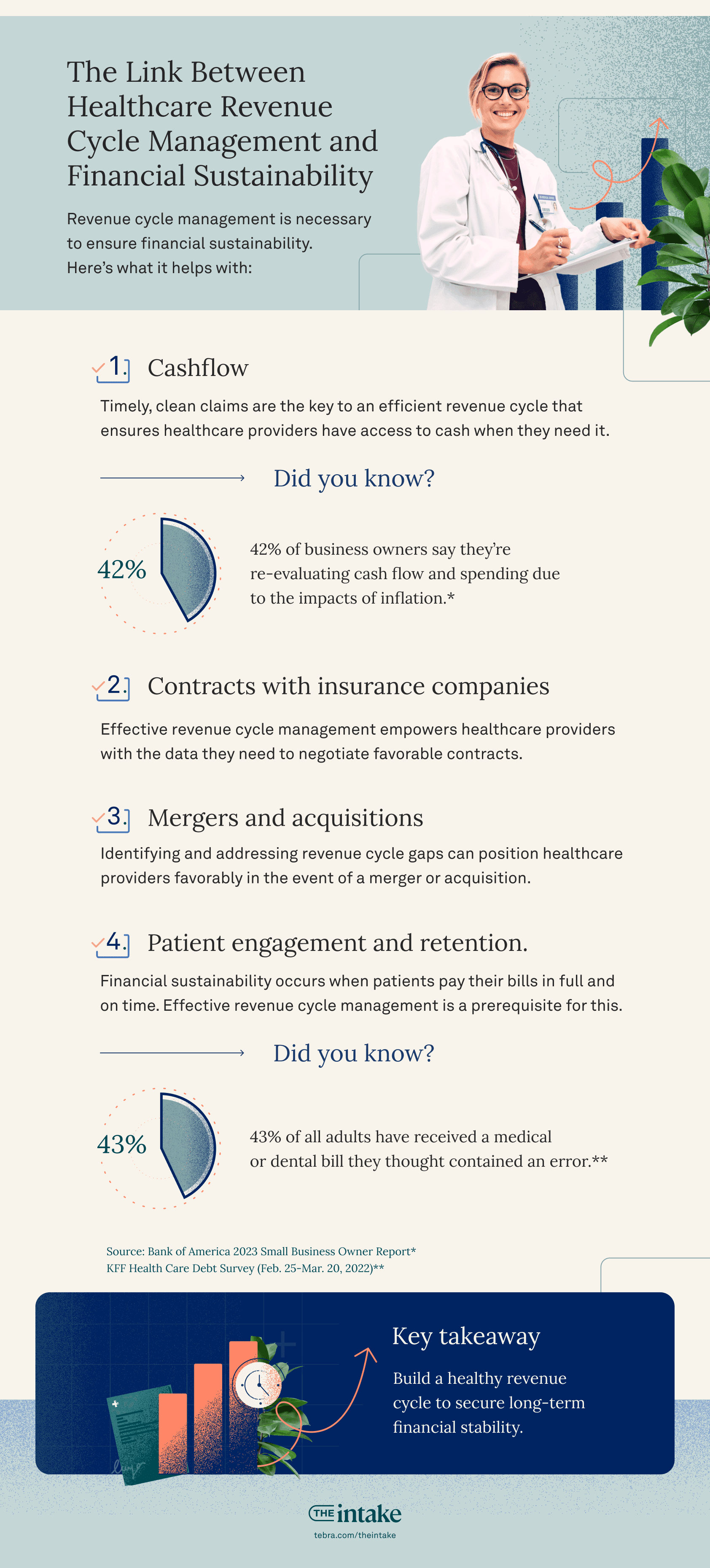
Revenue cycle management is necessary to ensure financial sustainability because it helps with the following:
Cash flow
Poor cash flow management is one reason why small businesses fail.
In healthcare, good cash flow requires submitting accurate medical claims in a timely manner. Timely, clean claims are the key to a timely revenue cycle that ensures healthcare providers have access to cash when they need it.
Not surprisingly, 42% of business owners say they’re re-evaluating cash flow and spending due to inflation.
Contracts with insurance companies
Effective revenue cycle management empowers healthcare providers with the data they need to negotiate favorable contracts.
Mergers and acquisitions
Identifying and addressing revenue cycle gaps can position healthcare providers favorably in the event of a medical practice sale or merger.
Pro tip: During healthcare organization mergers and acquisitions, keep these revenue cycle management tips in mind:
- Monitor KPIs such as the denial rate, days in A/R, net collection rate, and clean claims rate.
- Conduct ongoing medical billing and medical coding audits before, during, and immediately after the transition.
- Consider fully outsourcing healthcare revenue cycle management or augmenting staff with an outsourced vendor.
- Focus on the patient experience. Let patients know what they can expect during the transition and how it benefits them.
- Prioritize change management to prevent costly staff turnover.
- Standardize medical coding and medical billing guidelines, policies, and workflows to ensure consistency and efficiency.
Patient engagement and retention
Financial sustainability occurs when patients pay their bills in full and on time. Effective revenue cycle management is a prerequisite for this. Why? 43% of adults say they have received a medical or dental bill they thought contained an error.
“43% of adults say they have received a medical or dental bill they thought contained an error. ”
About two-thirds of these adults say the error involved being billed for something that should have been covered by health insurance. Other errors were being billed for services never received or for bills that had already been paid.
Revenue cycle management prevents medical billing errors that can otherwise erode patient trust and delay patient payments, making it impossible to achieve financial sustainability.
What are some common revenue cycle management solutions?
There are many types of healthcare revenue cycle management solutions that can help health systems and medical practices thrive. Here are 5 categories of solutions and examples of technology that fit into each one:
- Billing and payments: Practice management software, insurance eligibility, patient statements, and patient payments
- Care delivery: EHRs and telehealth
- Data and insights: Medical practice growth analytics, medical practice revenue analytics, and data cloud
- Medical practice growth: Medical practice reputation management software
- Patient experience: Online scheduling, appointment reminders, patient intake, text messaging, and patient portals
How does billing software help with revenue cycle management?
Billing software benefits revenue cycle management because it relieves the administrative burden associated with eligibility and prior authorization. It also keeps the revenue cycle team up to date with payer policies and new medical codes, reduces turnaround time for patient payments, and more.
What is the best way to measure the effectiveness of healthcare revenue cycle management?
KPIs are the best way to measure revenue cycle management effectiveness. Data will reveal areas where healthcare providers are performing well and areas where they need to improve. Here are few of the most important KPIs:
- Avoidable write-offs as a percentage of revenue
- Bad debt
- Clean claims rate
- Days in accounts receivable
- Days in discharge not final billed
- Denials
- Medical coding and medical billing productivity
- Missed charges
- Overall medical coding accuracy
- Point of service cash collections
- Underpayment recoveries
What should healthcare providers keep in mind about revenue cycle management moving forward?
Like many aspects of healthcare, revenue cycle management is constantly evolving. However, there are several trends worth noting. These include:
- Continued focus on the patient experience. This includes the clinical experience as well as the financial one. Patients will increasingly want seamless and convenient scheduling, treatment, and payment options.
- Persistent revenue cycle management staffing shortages. Staffing shortages may continue to challenge healthcare providers. Partnering with outsourced vendors, leveraging automation, or finding other creative ways to address shortages (e.g., grow your own medical coders or share resources with other medical practices) will be paramount.
- Push for price transparency. As patients become more aware of the cost of their care, they may be more selective in choosing providers based on price. Medical practices must provide high-quality care at the lowest price to attract and retain patients.
- Shift toward value-based care. The link between reimbursement, quality of care, and patient outcomes will only become more apparent in the years ahead. Medical practices must promote strategic alignment between revenue cycle management, innovative payment models, and value-based care.
Revenue cycle management is an exciting and critical aspect of healthcare delivery. Medical practices prioritizing patient care's financial aspect will experience sustainability in the years ahead.
You might also be interested in
Optimize your private practice for growth. Get actionable strategies to create a superior patient experience, retain patients, and support your staff while growing your medical practice sustainably and profitably.