Get paid faster
Streamline your billing and collections processes to improve speed to revenue.

0 %
of providers take 30+ days to collect after a patient encounter
0 %
of providers rely on manual and paper-based transactions to collect
0 %
of consumers prefer an electronic payment method for medical bills
Simplify the process of getting paid
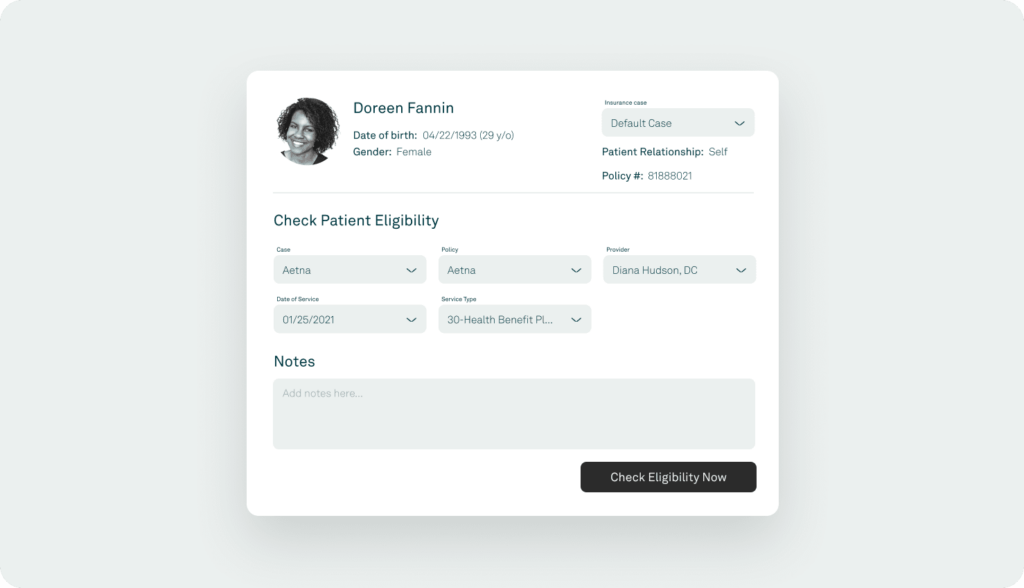
Insurance eligibility checks and patient authorizations
Easily submit insurance eligibility inquiries to thousands of government and commercial insurance companies, save details for future reference, run daily batch checks, and verify patient eligibility with visual icons.
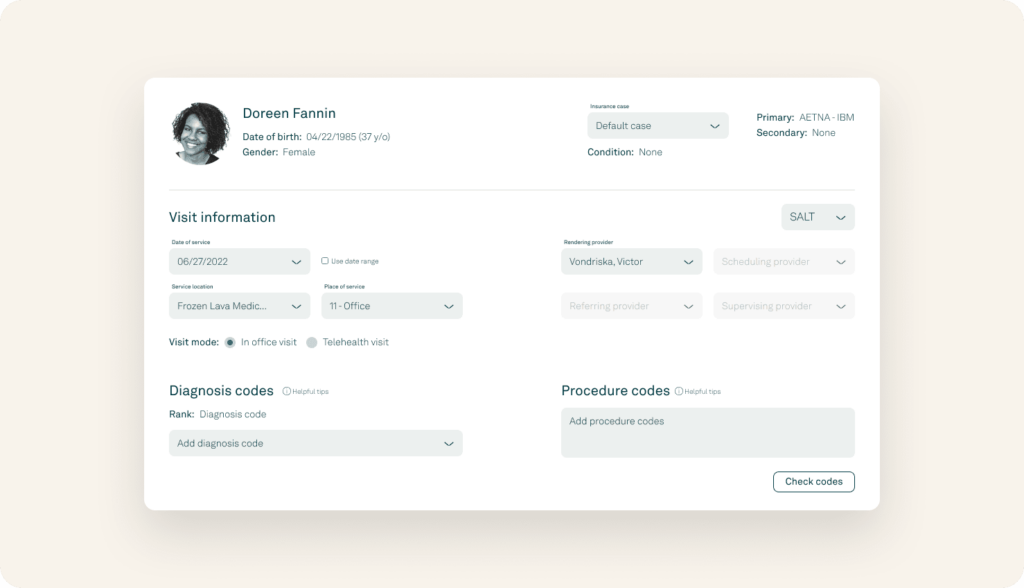
Charge capture
Tebra makes entering changes quick and easy. Add procedure codes from saved code favorites lists or new searches. Plus, add modifiers to optimize workflows. Reduce redundant data entry to refocus your time on higher-impact activities.
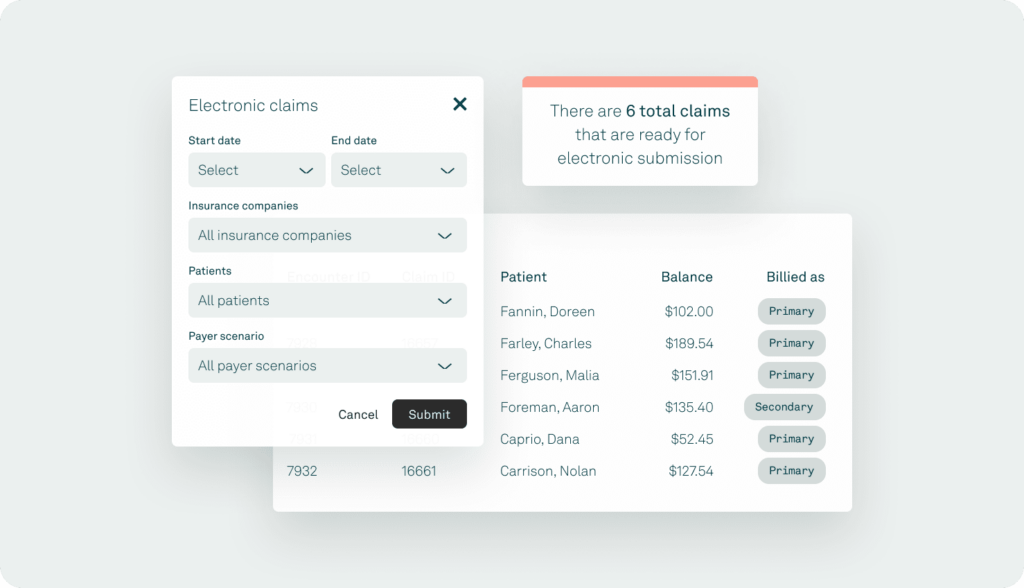
Claims submission and management
Send electronic claims to more than 8,000 government payers and commercial insurance companies, print paper claims when necessary, and receive claim processing reports with status updates. Get paid faster from insurance companies and avoid costly delays and cash flow disruptions.
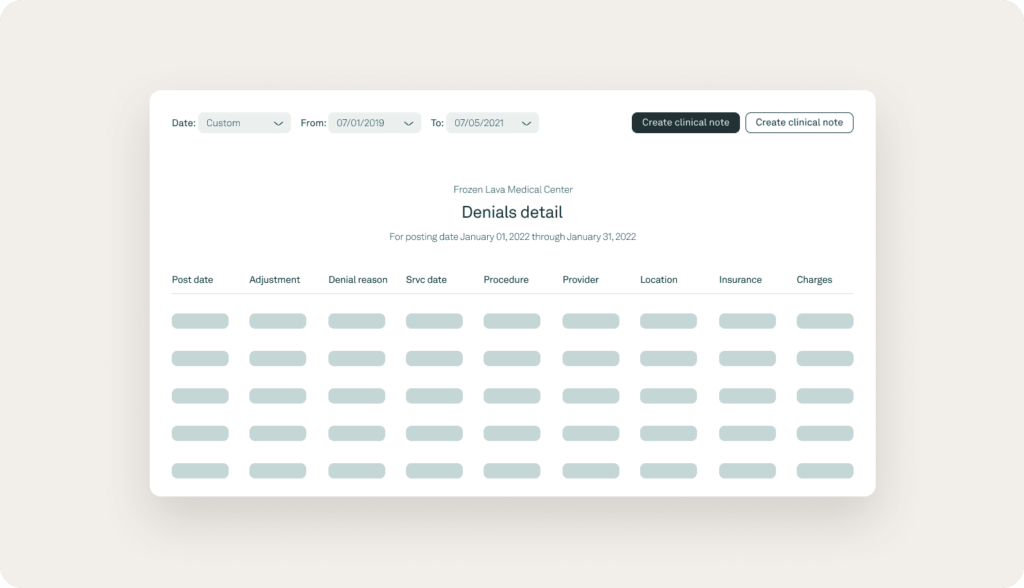
Rejection and denial management
Address the root cause of your denials so you can reduce the number you encounter on a daily basis. Billers can automatically flag denials that require review, efficiently resolve denials, and resubmit insurance claims.
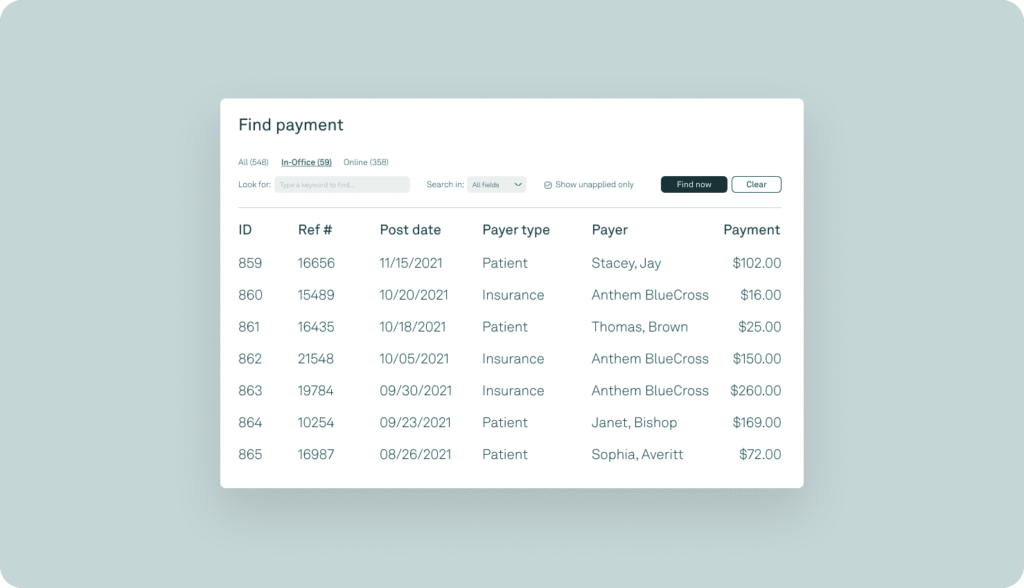
Payment posting
Improve your productivity, get paid faster, and easily reconcile your patient accounts with automatic posting for electronic insurance payments.
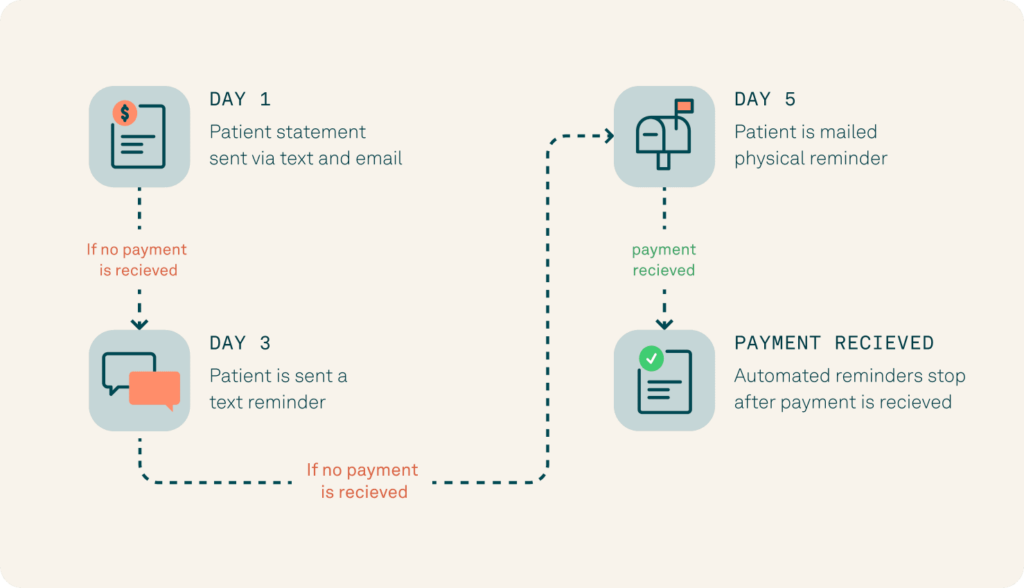
Automated patient billing
Pre-programmed text, email, and mailed statements simplify your patient collections workflow and ensure you communicate in the right way at the right time.
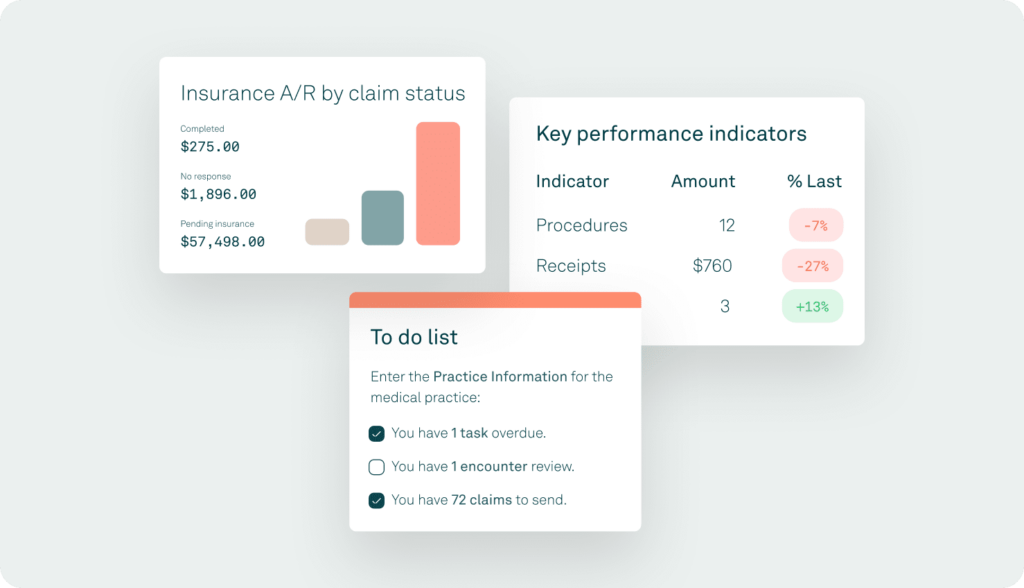
A/R management
Reduce days in accounts receivable with our comprehensive end-to-end claim tracking, available in both the enterprise and web applications.




